When a pharmacy technician pulls a bottle off the shelf, they’re not just grabbing a pill-they’re handling a patient’s life. In the U.S., 90% of prescriptions filled are for generic drugs. That means if a tech can’t tell the difference between metformin and Glucophage, or confuse hydroxyzine with hydralazine, they’re putting someone at risk. This isn’t theoretical. The Institute for Safe Medication Practices reports that 10-15% of medication errors tied to generic-brand confusion lead to serious harm or death. Training pharmacy technicians to master generic drug competency isn’t optional-it’s the bedrock of safe pharmacy practice.
Why Generic Drug Knowledge Is Non-Negotiable
Generic drugs are chemically identical to their brand-name counterparts, but they’re cheaper, widely used, and often substituted without the prescriber’s direct involvement. Pharmacy technicians are the first line of defense in making sure that substitution happens correctly. If a technician misreads a generic name, dispenses the wrong strength, or fails to recognize a therapeutic duplication (like giving two different generics for the same condition), the consequences can be deadly. The data is clear: technicians who score below 70% on generic drug identification tests make 3.2 times more dispensing errors than those who score above 90%. A 2023 study from the University of Utah tracked 1,247 technicians across 42 pharmacies and found that those with weak generic drug knowledge were far more likely to hand out the wrong medication-even when the prescription was written correctly. The problem isn’t just about names. It’s about shapes, colors, imprints, and dosages. One tech in Ohio accidentally gave a patient a 10mg tablet of glipizide thinking it was glyburide. Both are diabetes drugs, both are round and white. The patient went into hypoglycemic shock.What the Standards Actually Require
The Pharmacy Technician Certification Board (PTCB) sets the gold standard. Their 2026 exam now dedicates 18% of its content to generic drug knowledge-up from 14% in 2023. Technicians must be able to:- Match at least 200 commonly prescribed medications by generic and brand name
- Identify drug classifications (e.g., statins, SSRIs, ACE inhibitors)
- Recognize therapeutic duplications
- Understand dosage forms and routes of administration
- Know high-alert medications like insulin, anticoagulants, and opioids by both names
How Training Programs Are Adapting
Most community college pharmacy tech programs now include 35-40 hours of dedicated drug name training within their 1,200-hour curriculum. The most effective programs don’t rely on rote memorization. They use systems:- Grouping by therapeutic class: Instead of memorizing atorvastatin, simvastatin, and rosuvastatin as separate items, techs learn them all as “statins” used for cholesterol. This helps them predict what’s likely to be prescribed and spot duplicates.
- Visual association: Many techs swear by learning drugs by appearance-color, shape, imprint. A blue, oval pill with “50” on one side? That’s sertraline. A white, round tablet with “10” and a line? That’s metoprolol. Reddit user “GenericGuru” says this method cut their study time in half.
- Flashcards with clinical context: Don’t just write “lisinopril = Zestril.” Write: “Lisinopril (Zestril)-ACE inhibitor, used for HTN and heart failure, watch for cough and angioedema.” Context sticks better than names alone.

The Biggest Pitfalls and How to Avoid Them
Even well-trained techs stumble on look-alike, sound-alike (LASA) drugs. The ISMP tracks 37 dangerous pairs:- Hydroxyzine (allergy) vs. Hydralazine (blood pressure)
- Glipizide (diabetes) vs. Glyburide (diabetes)
- Clonazepam (seizures) vs. Clonidine (HTN)
- Levothyroxine (thyroid) vs. Levofloxacin (antibiotic)
What’s Changing in 2025 and Beyond
The field is evolving fast. In 2025, the VA rolled out mandatory quarterly assessments. The PTCB added biosimilars to its exam-those are complex biologic drugs that mimic brand-name biologics like Humira. Technicians now need to understand that adalimumab-atto is a biosimilar to Humira, not a generic. The FDA approves 15-20 new generic drugs every month. No static list can keep up. That’s why forward-thinking programs are shifting from memorizing names to teaching how to learn. Instead of asking, “What’s the brand name for metformin?” they’re asking, “How would you find the brand equivalent if you don’t know it?” The future of competency isn’t just about knowing 200 drugs. It’s about knowing how to navigate change. Techs who can use resources like the FDA Orange Book, consult pharmacists quickly, and double-check formularies will be the ones who stay ahead.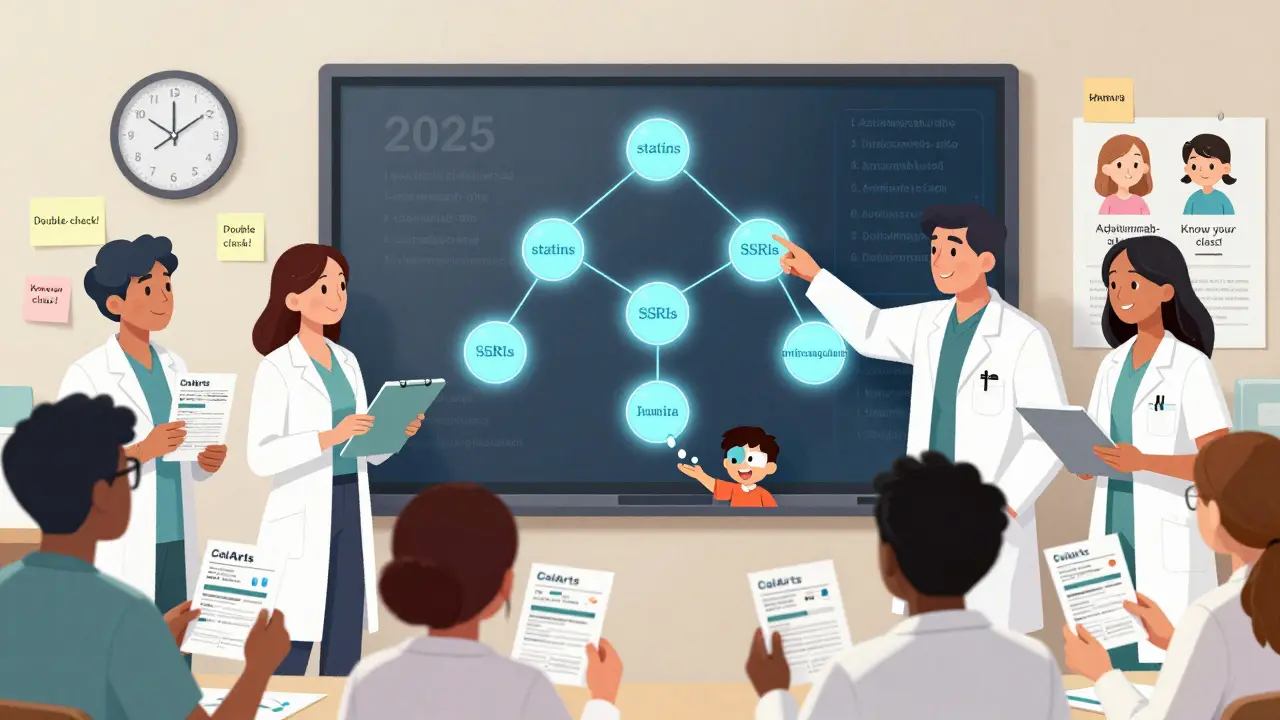
What You Can Do Right Now
If you’re a pharmacy tech, here’s your action plan:- Get the PTCB’s Top 200 Drug List. Focus on the first 100-those make up 80% of prescriptions.
- Group them by class: antihypertensives, antidepressants, antibiotics, etc.
- Use flashcards with images of the pills. Apps like RxTechExam or PTCB Test Prep have built-in image libraries.
- Practice daily: Spend 15 minutes a day quizzing yourself on 5 drugs. Use the “name → class → use → side effect” format.
- Find a study buddy. Explain each drug out loud. Teaching forces you to understand it.
Final Thought: It’s Not About Memorization-It’s About Safety
Generic drugs save the U.S. healthcare system billions every year. But they only work if the right one gets to the right patient. Pharmacy technicians aren’t just order-fillers. They’re medication safety officers. Mastering generic drug names isn’t a test you pass-it’s a habit you build. And every time you get it right, you’re preventing a mistake that could cost someone their health-or their life.Why are generic drugs so important in pharmacy practice?
Generic drugs make up 90% of all prescriptions filled in the U.S. They’re cheaper, just as effective as brand-name versions, and are often substituted automatically by pharmacies. This saves patients money and reduces healthcare costs. But for this system to work safely, pharmacy technicians must accurately identify and dispense them. Mistakes in generic drug identification lead to medication errors, which can cause serious harm or death.
What’s the difference between a generic drug and a brand-name drug?
A generic drug has the same active ingredient, strength, dosage form, and route of administration as the brand-name drug. It’s approved by the FDA as bioequivalent-meaning it works the same way in the body. The only differences are the inactive ingredients (like fillers or dyes), packaging, and price. Generics cost 80-85% less than brand-name versions. For example, metformin is the generic for Glucophage.
How many generic drugs should pharmacy technicians know?
The PTCB certification exam requires knowledge of at least 200 commonly prescribed medications by both generic and brand name. Most training programs focus on the Top 200 list, with emphasis on the Top 100, which account for over 80% of prescriptions. In hospital settings, especially the VA, technicians must know 300+ drugs, including all controlled substances.
What are look-alike, sound-alike (LASA) drugs, and why are they dangerous?
LASA drugs have names or appearances that are easily confused. Examples include hydroxyzine (for allergies) and hydralazine (for high blood pressure), or glipizide and glyburide (both for diabetes). Mixing them up can cause serious harm-like giving a blood pressure drug to someone with anxiety, or doubling up on diabetes meds. The Institute for Safe Medication Practices lists 37 high-risk LASA pairs. Always double-check spelling, pronunciation, and pill appearance.
Is memorizing drug names enough to be competent?
No. Memorization is a starting point, but true competency means understanding drug classes, therapeutic uses, side effects, and potential interactions. A tech who knows that lisinopril is an ACE inhibitor used for high blood pressure can infer that other ACE inhibitors like enalapril or ramipril serve similar purposes. This helps spot therapeutic duplication and reduces errors when new generics enter the market. Experts now recommend learning by class, not just by name.
How often do generic drug names change?
The generic drug name itself doesn’t change-it’s standardized by the FDA. But the manufacturer, packaging, pill shape, color, or imprint can change frequently. About 15-20 new generic versions enter the market every month. A tech who learned metformin from one manufacturer might see a different-looking pill from another. That’s why it’s critical to check the label for manufacturer and lot info, not just the name.






10 Comments
This is why I quit my job at the CVS drive-thru
One day I handed a patient metformin thinking it was glyburide and they looked at me like I just handed them a snake
Turns out I mixed them up because both were white round pills
My manager said 'just scan it' but the scanner failed
Now I study 15 mins a day with flashcards and I swear by it
I don't care if it's boring I'd rather be alive than guilty
Also if you're not using RxTechExam you're doing it wrong
The PTCB standards are too weak. If you can't name 300 drugs cold you shouldn't be touching prescriptions. The VA gets it right. No excuses. No exceptions. No 'I thought it looked similar.' People die because techs are lazy. Fix the training or get out of the way.
Therapeutic class grouping is the only valid pedagogical approach. Memorizing individual drug names is cognitively inefficient and brittle under pressure. The cognitive load theory supports chunking by pharmacodynamic class-statins, SSRIs, ACEi-which enables schema-based recognition. High-alert medications require additional encoding via visual imprint and manufacturer metadata. The 2026 PTCB exam reflects this shift. If your program still uses rote flashcards without clinical context, you're training for failure.
This is so important. I'm from India and we don't have brand-name drugs much here. Everyone uses generics. But I've seen pharmacists mix up names too. I wish more places trained like this. It's not just about rules-it's about care. Small things like checking the imprint can save lives.
Why are we letting foreign countries dictate our standards? The VA does it right. Why can't the whole country follow? We’re the best healthcare system in the world. Stop being lazy. Learn the drugs or get a different job.
They're hiding something. Why are there so many look-alike drugs? Coincidence? Or is Big Pharma intentionally making names confusing so we need more techs? And why does every generic look different now? 🤔 They're testing us. They want us to fail so they can push more brand-name stuff. I'm not taking any pills until I verify the imprint with 3 sources. 🚨
I used to dread studying drug names. Then I started teaching my roommate. Explaining lisinopril out loud made me remember its side effects. Now I quiz my coworkers during coffee breaks. It’s not about being perfect-it’s about being careful. One less mistake means one more person goes home safe.
It’s not just about memorization-it’s about contextual fluency. The cognitive architecture required for accurate generic identification involves pattern recognition across multiple modalities: orthographic (name), visual (imprint, color), phonological (pronunciation), and semantic (class, use). The failure modes are not random; they cluster around LASA pairs with high phonological overlap. Training must therefore be multimodal, iterative, and reinforced through spaced repetition. The PTCB’s 2026 update is a step forward, but institutional adoption remains fragmented. We need standardized, competency-based assessments-not just checklists.
In Nigeria, we use generics because we have to. No one can afford brands. So we learn fast. Color, shape, imprint. Always check. Never assume. One mistake here can kill someone with no backup. This post? It’s not American-it’s universal.
Who wrote this? Pharma shill? 90% generics? Yeah right. The FDA approves 15 new generics a month? More like 15 new ways to confuse you. And those AI training apps? They're tracking you. They know which drugs you mess up. They're building a profile. Next thing you know, your insurance denies your meds because 'you're a high-risk tech.' Wake up. This isn't training. It's control.