When you're trying to get pregnant, already pregnant, or breastfeeding, the medications you take - even the ones you think are harmless - can have real effects on your body and your baby. Yet, many women walk into their OB/GYN appointments without a clear list of what they’re taking, assuming their doctor will know or that supplements don’t count. That’s a mistake. Medication safety during pregnancy and breastfeeding isn’t optional. It’s essential. And the better prepared you are, the safer and more effective your care will be.
Why This Conversation Matters More Than You Think
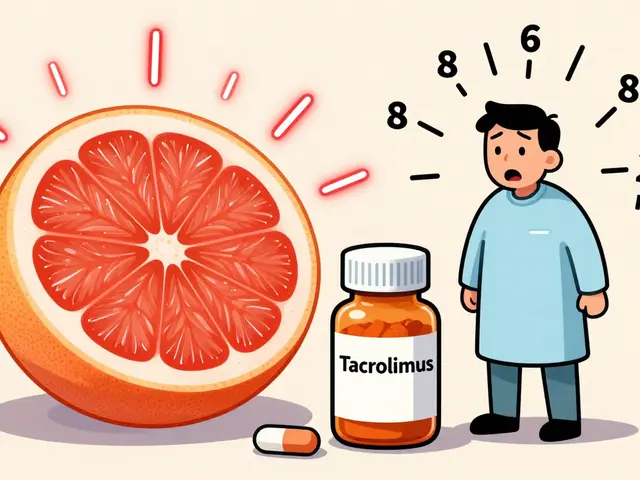
Nearly 90% of pregnant women in the U.S. take at least one medication during pregnancy, according to the CDC. That includes prescription drugs, over-the-counter pain relievers, vitamins, herbal teas, and even CBD oil. But not all of them are safe. Some can interfere with fetal development, affect breast milk production, or interact dangerously with other meds you’re on. Your OB/GYN isn’t just checking your blood pressure or listening to the baby’s heartbeat. They’re also doing a safety audit of everything you’re putting into your body. This isn’t about judging you. It’s about preventing harm. For example, ibuprofen might seem like a harmless headache remedy, but it can reduce amniotic fluid levels in the third trimester. St. John’s Wort, often taken for mood support, can cut the effectiveness of birth control pills by half. And if you’re using medical marijuana - which 18% of reproductive-age women do, according to the National Survey on Drug Use and Health - your provider needs to know. Most don’t ask unless you bring it up.What to Bring to Your Appointment
Don’t rely on memory. Write it down. Here’s exactly what you need to list:- Prescription medications: Name, dose, frequency, and reason. Don’t say “I take my thyroid pill.” Say: “Levothyroxine 75 mcg, one tablet daily, for hypothyroidism.”
- Over-the-counter drugs: Painkillers, antacids, cold meds, sleep aids. Include brand and generic names. “Tylenol 500mg, two tablets every 6 hours as needed for headaches.”
- Supplements and vitamins: Prenatal vitamins, iron, calcium, omega-3s - even if they’re labeled “natural.” Include brand names. “Nature Made Prenatal, one tablet daily.”
- Herbal products and teas: Chamomile, ginger, red raspberry leaf, echinacea. These aren’t harmless. Red raspberry leaf can stimulate contractions. Ginger is generally safe, but high doses may affect blood clotting.
- Recreational substances: Alcohol, nicotine, cannabis, and even vaping. Be honest. Your provider isn’t there to shame you - they’re there to help you stay safe.
Pro tip: Take a photo of each pill bottle or box. You can show it to your provider on your phone. This helps avoid mix-ups, especially if you take multiple pills that look alike.
What Your OB/GYN Is Looking For
Your provider isn’t just collecting a list. They’re evaluating risk. They use a system called pregnancy safety categories (A, B, C, D, X) to guide decisions. Category A means proven safe in human studies (rare). Category B means no evidence of harm in studies. Category C means animal studies showed risk, but human data is limited. Category D means there’s clear risk, but benefits may outweigh it. Category X means clear risk and the dangers outweigh any benefit. For example:- Safe during pregnancy: Folic acid (400-800 mcg daily), prenatal vitamins, levothyroxine, insulin, certain blood pressure meds like labetalol and nifedipine.
- Use with caution: Most antidepressants (SSRIs like sertraline), certain antibiotics (azithromycin), and antihistamines (loratadine).
- Generally avoided: Ibuprofen (after 20 weeks), isotretinoin (Accutane), lithium (in high doses), and ACE inhibitors like lisinopril.
For breastfeeding, the rules are slightly different. Most medications pass into breast milk in tiny amounts. But some can affect milk supply or the baby’s development. For instance, pseudoephedrine (in Sudafed) can reduce milk production. Benzodiazepines like lorazepam can make babies sleepy. Your OB/GYN will help you find safer alternatives.

What Questions to Ask
Don’t just listen - ask. Here are the most important questions to bring:- “Is this medication safe for pregnancy and breastfeeding?”
- “Is there a safer alternative I could use instead?”
- “Should I stop this before I get pregnant, or can I keep taking it?”
- “Will this affect my fertility or chances of conceiving?”
- “What should I do if I accidentally took something unsafe?”
- “Do I need to change my dosage now that I’m pregnant?”
Also ask: “Can you write down what I should stop, start, or change?” Many patients forget what they’re told. A written note or printed handout helps.
Common Mistakes Women Make
You’re not alone if you’ve made one of these mistakes:- Thinking “natural” means safe. Herbal teas, essential oils, and supplements aren’t regulated like drugs. They can still be harmful.
- Forgetting to mention what you take occasionally. “I only take Advil when I have a bad headache” - that still matters.
- Waiting until you’re pregnant to talk about meds. The best time to review medications is before you try to conceive. That’s when changes have the biggest impact.
- Not telling your provider about your mental health meds. Depression and anxiety are common during pregnancy. Untreated, they can be riskier than the meds used to treat them.
One patient on Reddit shared that she brought a spreadsheet with every supplement she took - including brand names and doses - and her OB printed it to keep in her file. Another forgot to mention evening primrose oil and found out too late that it could trigger early labor. The difference? Preparation.
What to Do If You’re Already Pregnant
If you’re already pregnant and haven’t reviewed your meds yet - don’t panic. Just schedule an appointment. Don’t stop anything suddenly unless your provider says so. Some meds, like thyroid pills or antidepressants, need to be adjusted, not stopped. Abruptly stopping them can be more dangerous than continuing them. Your provider may suggest switching to a pregnancy-safe version. For example, if you’re on a statin for cholesterol, you’ll likely switch to diet and exercise until after delivery. If you’re on a blood pressure med like lisinopril, you’ll probably switch to labetalol or nifedipine.
How to Stay on Track After Your Appointment
Once you’ve had the conversation, write down the changes:- What to stop
- What to start
- What dose to change
- When to check back
Set a reminder on your phone for 2 weeks later: “Check if I’m taking the right meds.” Many women forget what they were told after a few days. A quick review saves stress later.
Also, update your list every time you get a new prescription or change your routine. If you start a new supplement or stop a medication, tell your OB/GYN the next time you see them - even if it’s just a routine checkup.
What’s New in 2026
In 2023, the American College of Obstetricians and Gynecologists updated its guidelines to require detailed discussions about CBD and medical marijuana. More clinics are now using digital tools to track medication use. For example, GW Medical Faculty Associates launched a mobile app that lets pregnant patients log their blood pressure meds in real time - and 89% of users stick with it. By 2024, the FDA plans to roll out standardized pregnancy risk scores for medications - a simple 1-5 scale that tells you how risky a drug is during pregnancy. And ACOG is releasing an official patient checklist app in Q2 2024 to help women prepare for their visits.Final Thought: You’re the Expert on Your Body
Your OB/GYN has the medical training. But you have the lived experience. You know what you take, how you feel, and what you’re comfortable with. Bring your list. Ask your questions. Push for clarity. If your provider rushes you or dismisses your concerns, it’s okay to ask for more time or a second opinion. The goal isn’t to eliminate all medications. It’s to make sure the ones you take are the right ones - at the right time - for you and your baby.Should I stop all my medications when I get pregnant?
No. Many medications are safe and necessary during pregnancy. Stopping them suddenly can be more dangerous than continuing them. For example, stopping thyroid medication can harm fetal brain development. Always talk to your OB/GYN before making changes.
Are prenatal vitamins enough, or do I need other supplements?
Prenatal vitamins cover key nutrients like folic acid, iron, and DHA, but you may need more depending on your health. If you’re low in vitamin D, have anemia, or are vegetarian, your provider might recommend extra iron, calcium, or B12. Never add supplements without checking first - some can interfere with absorption or cause toxicity.
Can I take ibuprofen while breastfeeding?
Ibuprofen is generally considered safe in small doses while breastfeeding. It passes into breast milk in very small amounts and is unlikely to affect your baby. However, avoid long-term use or high doses, and always check with your provider if you’re taking it regularly.
What if I took something unsafe before I knew I was pregnant?
Tell your OB/GYN right away. Most exposures in early pregnancy don’t cause harm. The critical window for major birth defects is between weeks 3 and 8. Your provider can assess the risk based on the drug, timing, and dosage. In most cases, there’s no need for panic - just awareness and monitoring.
Why does my OB/GYN care about my herbal tea?
Herbal teas aren’t regulated like drugs, so their ingredients and potency can vary. Some, like red raspberry leaf, can stimulate uterine contractions. Others, like licorice root, can raise blood pressure. Even “harmless” teas can interact with medications or affect hormone levels. Your provider needs to know so they can spot risks.
Do I need to tell my OB/GYN if I use cannabis for anxiety?
Yes. Cannabis use during pregnancy is linked to lower birth weight and developmental delays. Even if you use it for anxiety, your provider needs to know to help you find safer alternatives - like therapy, exercise, or pregnancy-safe medications. They won’t judge - they’ll help.