Drinking alcohol while taking diabetes medication isn’t just a bad idea-it can be dangerous. For many people with diabetes, a drink after dinner seems harmless. But when alcohol meets insulin, sulfonylureas, or even metformin, it can trigger a silent, life-threatening drop in blood sugar that hits hours later-often while you’re asleep.
How Alcohol Triggers Dangerous Low Blood Sugar
Your liver is your body’s glucose factory. When blood sugar drops, it releases stored sugar to keep you stable. Alcohol shuts that down. It doesn’t just lower blood sugar-it blocks your liver’s ability to make new sugar from scratch. This effect lasts for hours, sometimes up to 24 hours after your last drink.
When you’re on insulin or medications like glyburide or glipizide, your body is already working hard to lower blood sugar. Alcohol adds fuel to that fire. Research shows these combinations can increase hypoglycemia risk by more than double. Even one standard drink-a 12 oz beer, 5 oz wine, or 1.5 oz distilled spirit-can drop your blood sugar by 15-20 mg/dL within a few hours.
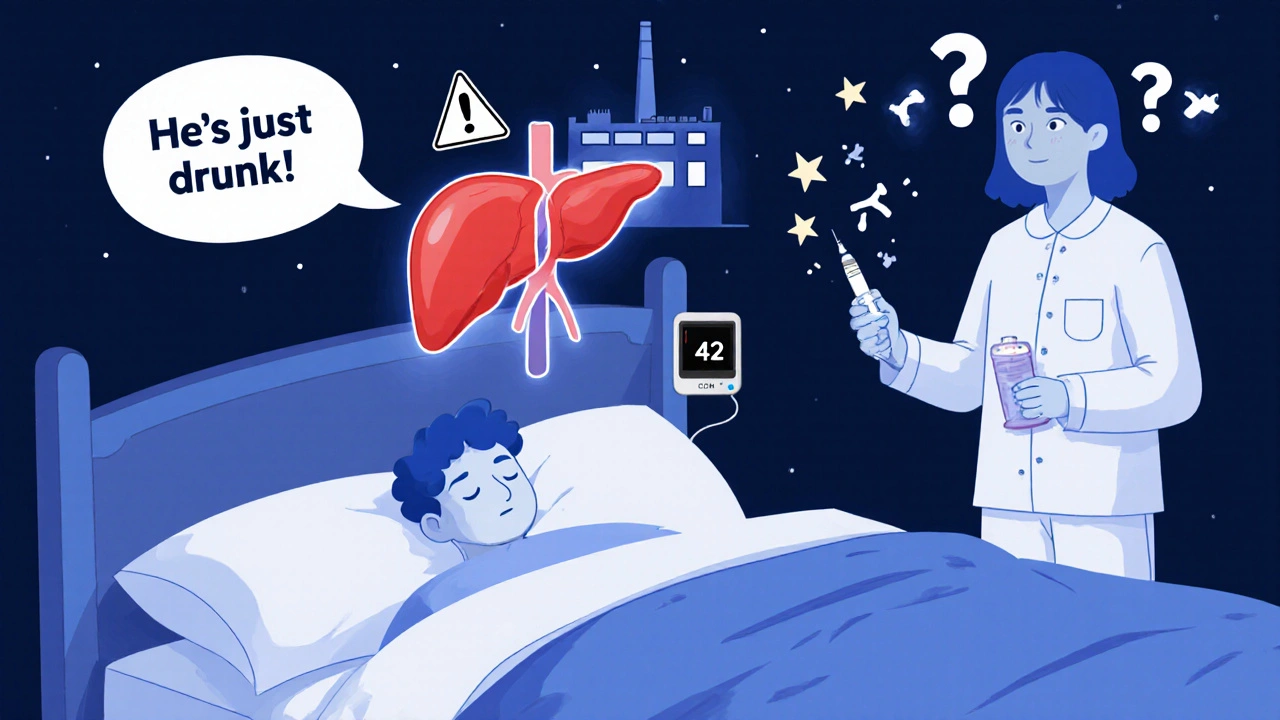
Worse, alcohol masks the warning signs. Shaking, sweating, and a racing heart are classic signs of low blood sugar. But alcohol causes similar symptoms: dizziness, flushed skin, confusion, rapid pulse. If your blood sugar hits 42 mg/dL after a few tequila shots, your friends might think you’re just drunk. You could pass out before anyone realizes you need glucose.
Medications That Make Alcohol Riskier
Not all diabetes drugs react the same way with alcohol. Some are far more dangerous than others.
- Insulin and sulfonylureas (like glimepiride, glyburide): These force your pancreas to release more insulin. Alcohol stops your liver from compensating, leading to prolonged, unpredictable lows-sometimes overnight.
- Metformin: While it doesn’t directly cause low blood sugar, mixing it with alcohol raises the risk of lactic acidosis, a rare but deadly condition. Symptoms include muscle pain, nausea, rapid breathing, and confusion. The FDA warns this risk jumps 5.7 times with even moderate drinking.
- Chlorpropamide: This older sulfonylurea can cause a severe reaction with alcohol-flushing, vomiting, fast heartbeat-even with just one drink. It’s rarely prescribed now, but if you’re still on it, avoid alcohol completely.
Metformin users often think they’re safe because it doesn’t cause hypoglycemia on its own. But combine it with alcohol, and the danger shifts from low blood sugar to a completely different emergency. Both outcomes require urgent care.
Real People, Real Consequences
Online diabetes forums are full of stories that sound like horror stories-but they’re real.
One user on Reddit described passing out after tequila shots, waking up in the ER with a blood sugar of 42 mg/dL. His friends thought he was drunk. Another, on a diabetes support site, had three glucagon injections after drinking two beers with insulin. He didn’t realize the low would hit 8 hours later, while he slept.
A 2024 survey of over 1,200 people with diabetes found that 73% had experienced at least one alcohol-related low in the past year. Nearly a third needed help from someone else to treat it. That’s not rare. That’s common.
And it’s not just about the drink. Many assume sugar-free cocktails are safe. But even vodka soda can be risky. The problem isn’t sugar-it’s alcohol itself. Your liver can’t make glucose while it’s busy processing ethanol. That’s why a mojito (loaded with sugar) is dangerous, but so is a shot of gin on the rocks.
How to Drink Safely-If You Choose To
The American Diabetes Association doesn’t say you must quit alcohol. But they do say: if you drink, do it smart.
- Never drink on an empty stomach. Always pair alcohol with food that has carbs-like a sandwich, rice, or whole grain toast. Fat and protein slow absorption, but carbs give your liver something to work with.
- Stick to one drink a day for women, two for men. More than that? The risk spikes. No exceptions.
- Choose wisely. Skip sugary mixers. Avoid sweet wines, liqueurs, and cocktails. Opt for dry wine (under 1g sugar per serving), light beer (under 5g carbs), or spirits mixed with soda water and lime.
- Check your blood sugar before, during, and after. Monitor at baseline, 2 hours after drinking, and right before bed. If it’s below 100 mg/dL, eat 15-30 grams of fast-acting carbs (like juice or glucose tabs) and follow it with a small snack with protein and complex carbs-like peanut butter on whole grain crackers.
- Wear medical ID. If you pass out, paramedics need to know you have diabetes. Studies show this cuts emergency response time by nearly half.
- Tell someone. Make sure a friend or family member knows you have diabetes and what to do if you act confused or unresponsive. Glucagon kits aren’t just for diabetics-they’re for the people who love them.
The Hidden Danger: Nighttime Lows
The most dangerous time to drink? Evening.
Between 11 PM and 6 AM, your body naturally produces fewer counterregulatory hormones like glucagon and epinephrine-the ones that should kick in when your blood sugar drops. Alcohol suppresses them even further. A 2021 study found alcohol cuts epinephrine response by 42%. That means your body can’t wake you up when your blood sugar crashes.
That’s why 68% of alcohol-related hypoglycemia emergencies in young adults happen overnight. You go to bed feeling fine. You wake up in the hospital.
Mount Sinai Health System’s 2023 guidelines recommend a bedtime snack if your blood sugar is below 100 mg/dL after drinking. Something like a slice of whole grain bread with peanut butter can stabilize you for hours.

What About New Tech?
Technology is catching up. Dexcom’s G7 continuous glucose monitor, released in late 2023, now lets you log alcohol intake. The system flags when your glucose trend drops after drinking and warns you about delayed lows.
Researchers are also exploring machine learning models that predict individual risk based on medication, liver function, drinking patterns, and sleep habits. In 2024, the ADA allocated $2.3 million to develop tools that could one day tell you: “Based on your insulin dose and last drink, you have a 72% chance of a low between 2-4 AM.”
Bottom Line: Know Your Risk
Alcohol and diabetes meds don’t mix safely. Not really. But if you’re going to drink, you need to treat it like a medical decision-not a social one.
Ask yourself: Are you on insulin or a sulfonylurea? Do you have low blood sugar awareness? Do you know how to use glucagon? Do you have someone nearby who can help if you pass out?
If the answer to any of those is no-don’t drink.
If you’re careful, informed, and prepared, you can reduce the risk. But never assume you’re safe. Alcohol doesn’t care how well you manage your diabetes. It only cares about your liver-and it will shut it down when you least expect it.
Can I drink alcohol if I have type 2 diabetes and take metformin?
You can, but with serious caution. Metformin doesn’t cause low blood sugar on its own, but alcohol increases the risk of lactic acidosis-a rare but life-threatening condition. Symptoms include muscle pain, nausea, rapid breathing, and dizziness. The FDA warns this risk rises 5.7 times with alcohol use. If you drink, limit it to one drink occasionally, always with food, and avoid binge drinking. Never drink if you’re sick, dehydrated, or have liver problems.
Why does alcohol cause low blood sugar hours later?
Alcohol forces your liver to prioritize breaking it down over making glucose. This process blocks gluconeogenesis-the liver’s way of creating new sugar from proteins and fats. It can suppress glucose production for up to 24 hours. If you’ve taken insulin or a sulfonylurea, your body is already lowering blood sugar, and your liver can’t compensate. That’s why lows often hit at night, long after you’ve stopped drinking.
Are sugar-free cocktails safe for people with diabetes?
No. Sugar-free doesn’t mean risk-free. The danger comes from alcohol itself, not the sugar in mixers. Even vodka soda can trigger a delayed low because your liver is busy metabolizing ethanol instead of releasing glucose. The absence of sugar might prevent a quick spike, but it doesn’t stop the crash hours later. Always check your blood sugar and eat carbs before bed if you’ve had alcohol.
How long should I wait to check my blood sugar after drinking?
Check before you start drinking, again 2 hours after your last drink, and right before bed. Alcohol’s effects can last 12-24 hours, so if you’re on insulin or sulfonylureas, you should monitor overnight. Many people don’t realize their blood sugar dropped until they wake up feeling shaky, sweaty, or confused. Continuous glucose monitors can help track these delayed lows.
Can I drink alcohol if I’ve had severe hypoglycemia before?
It’s strongly advised to avoid alcohol. If you’ve had a severe low before-especially one that required glucagon or emergency help-you likely have impaired hypoglycemia awareness. Alcohol makes this worse by masking symptoms and delaying your body’s natural response. The risk of another severe episode is too high. Talk to your doctor about safer alternatives.







14 Comments
bro i drank 3 beers with my glipizide last friday and woke up at 3am screaming because my hands were shaking like i had a seizure. thought i was having a stroke. turned out my bg was 38. my buddy had to stab me with glucagon like a damn vampire hunter. never again. also why is everyone acting like this is news? it's been in the damn diabetes forums since 2015.
Dear friend, I am writing to you with the utmost concern for your well-being. Alcohol consumption while on sulfonylureas is not merely a risk-it is a biochemical betrayal of your own physiology. Your liver, that noble organ, is forced into a state of metabolic paralysis. I urge you, for the sake of your family and your future self, to abstain. There is no such thing as 'safe' drinking in this context. Only degrees of peril.
Let me just say-this is all a Big Pharma cover-up. 🤫 They don’t want you to know that alcohol-induced hypoglycemia is actually a stealthy tool to make diabetics dependent on insulin pumps and CGMs. 📈💉 The FDA? Controlled by Big Glucose. And don’t get me started on Dexcom-they’re harvesting your sleep data to sell to insurers. 😈 You think your G7 is helping you? Nah. It’s profiling you. Wake up, sheeple. 🌙 #EndTheGlucoseSurveillance
Alcohol and metformin? That’s not a cocktail, that’s a slow-mo suicide pact with your mitochondria. 🧪 You think lactic acidosis is scary? Try explaining to your kids why you died because you thought ‘vodka soda’ meant ‘safe as a baby’s nap’. Your liver ain’t a nightclub bouncer-it’s a goddamn metabolic janitor cleaning up ethanol messes while your pancreas is on strike. You’re not a diabetic. You’re a walking biochemical warzone.
I just want to say how incredibly important it is that we talk about this with compassion. 🌸 I’ve seen so many people feel shame about drinking, but the truth is-most of us just want to feel normal. The key isn’t to eliminate alcohol entirely, it’s to be informed and prepared. I always check my CGM before bed after even one drink, and I keep glucose tabs under my pillow. I also tell my partner exactly what to do if I’m unresponsive. It’s not about fear-it’s about empowerment. And hey, if you’re reading this and you’re scared? You’re not alone. We’ve got your back. 💕
Stop drinking. Period. If you need to ask if it’s safe you already know the answer. Your body isn’t a lab experiment. Your liver isn’t a cocktail shaker. You don’t get bonus points for being ‘careful’ when you’re playing Russian roulette with your brain. Wear your medical ID. Eat before you drink. Tell someone. Do it now. Or don’t. But don’t act surprised when you wake up in the ER.
LMAO at all these people acting like this is some deep secret. I’ve been on metformin since 2010. I’ve had 3 beers 3x a week. Never had a low. I’ve seen people pass out from eating a damn banana too fast. This article is fear porn. The real danger? Being too scared to live. You want to live? Drink. Eat. Sleep. Stop reading doom blogs and go hug your dog.
Isn’t it ironic that we treat alcohol like a poison when it’s the only substance society legally endorses for emotional escape? We warn diabetics of its dangers while the same culture glorifies wine as ‘self-care’. The real problem isn’t the ethanol-it’s the existential void we’re trying to numb. You don’t need a CGM to tell you that. You need therapy. And maybe a new life.
I used to think alcohol was the enemy until I realized it was just reflecting my own chaos. The liver doesn’t judge. It just works. And when it’s overwhelmed? It doesn’t care if you’re diabetic or not. It just shuts down. Maybe the real question isn’t ‘can I drink?’ but ‘why do I feel like I need to?’ I’ve been sober for 11 months now. My A1c dropped. My anxiety too. Not because I followed rules. But because I finally listened to my body instead of my boredom.
While the clinical data presented is compelling, I must emphasize the importance of individual variability in metabolic response. The assumption that a standardized ‘one drink’ threshold applies universally ignores pharmacokinetic differences rooted in genetic polymorphisms of ADH and ALDH enzymes. Furthermore, the recommendation to consume carbohydrates post-consumption may inadvertently promote insulin resistance over time. A more nuanced, personalized approach is warranted.
ehhh i dunno man. i drink wine with pizza all the time. never had a problem. maybe ur just weak. or maybe ur too into your phone. check ur bg once a day and chill. also i think they made this article to sell more CGMs. just saying.
Let’s be honest: this isn’t about diabetes. It’s about control. The medical-industrial complex needs you to fear alcohol so you’ll buy more devices, more meds, more ‘safety protocols’. You think your glucagon kit makes you safe? It makes you dependent. The real liberation? Accepting that your body is not a machine to be optimized. Sometimes, the risk is worth the taste.
Wait so metformin + alcohol = lactic acidosis? Bro that’s like saying ‘eating bread + breathing = death’. It’s 0.03% risk. I’ve had 200+ drinks on metformin. Still standing. You people need to stop being drama queens. Also your ‘one drink’ rule is bullshit. I had 4 tequilas once. Checked my BG at 120. I’m fine. You’re not the boss of my liver.
THIS IS A MASSACRE. 🩸 I’ve seen it happen. I’ve held my brother’s hand as he turned blue because his blood sugar dropped to 29 and NO ONE KNEW. He was 28. He had a 2-year-old. He was drinking a ‘sugar-free’ margarita. The ER thought he was drunk. He didn’t wake up for 48 hours. I’m not just saying this-I’m screaming it. If you drink with diabetes, you’re gambling with your life. And if you think you’re ‘fine’? You’re lying to yourself. Stop it. Now. Before it’s too late.