Blood Thinner Decision Aid
Which blood thinner is safer for you?
Answer a few questions about your health to see if DOAC or warfarin is a better choice based on your unique risk factors.
Choosing a blood thinner isn’t just about preventing clots-it’s about living with the risks that come with it. For millions of people with atrial fibrillation, deep vein thrombosis, or pulmonary embolism, the choice between Direct Oral Anticoagulants (DOACs) and warfarin comes down to one thing: which one causes fewer serious side effects and fits better into real life?
What Are DOACs and How Do They Differ from Warfarin?
DOACs-like apixaban (Eliquis), rivaroxaban (Xarelto), dabigatran (Pradaxa), and edoxaban (Savaysa)-are newer blood thinners that target specific parts of the clotting process. Unlike warfarin, which blocks vitamin K to slow down multiple clotting factors, DOACs go straight for one target: either factor Xa or thrombin. This makes their action more predictable.
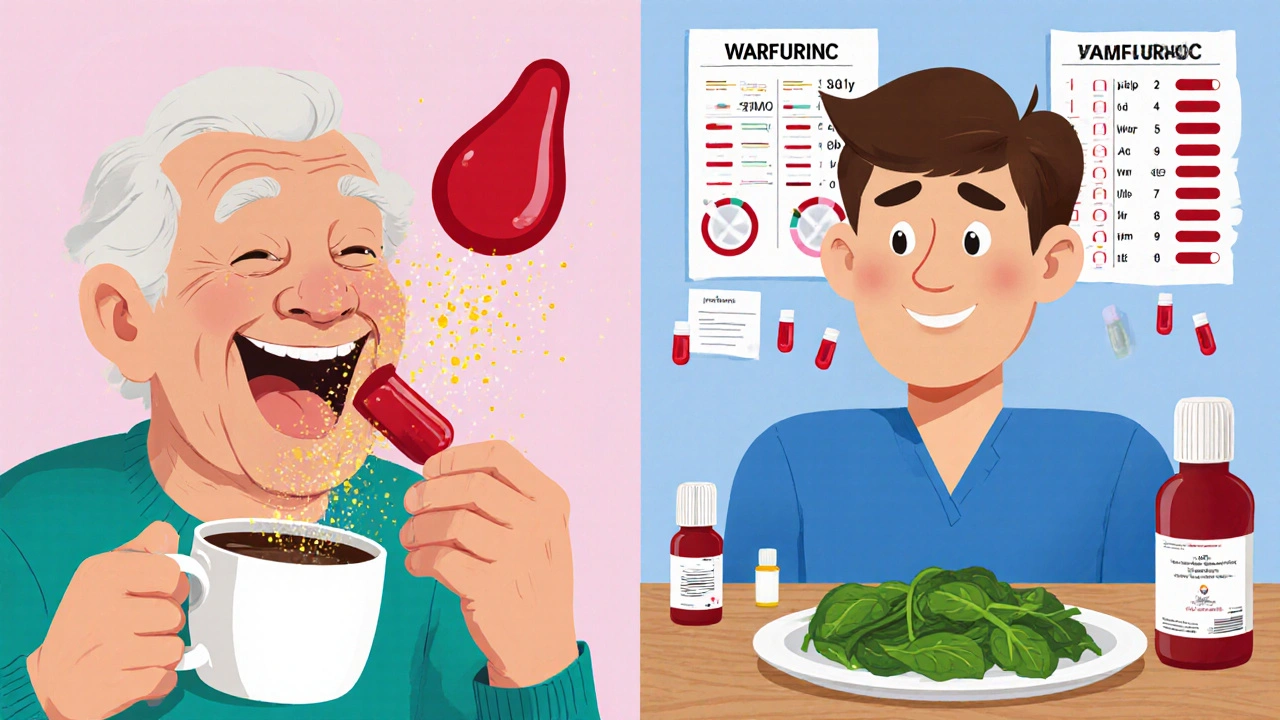
Warfarin has been around since the 1950s. It works, but it’s finicky. Your diet, other medications, even your genes can throw off its effect. That’s why people on warfarin need regular blood tests-INR checks-to make sure their dose is right. If the INR is too low, you’re at risk for a stroke. Too high, and you could bleed internally.
DOACs don’t need those tests. You take the same dose every day, no matter what you eat or what other pills you’re on. That’s a huge difference in daily life.
Bleeding Risks: The Biggest Concern for Both
The biggest danger with any blood thinner is bleeding. And when it comes to major bleeding-like bleeding in the brain, stomach, or intestines-DOACs win by a clear margin.
A 2023 study of nearly 18,500 patients found that those on DOACs had a 31% lower chance of being hospitalized for major bleeding than those on warfarin. That’s not a small edge. It’s life-changing.
Even more telling: DOACs reduce the risk of intracranial hemorrhage (bleeding in the brain) by 50-60%. Brain bleeds are often deadly or leave permanent damage. Warfarin carries a higher risk here because it’s harder to control. DOACs wear off faster, so if something goes wrong, the body can recover more quickly.
But not all DOACs are the same. Apixaban has the lowest bleeding rate among them-just 1.9 events per 100 people each year. Rivaroxaban is higher, at 2.8. Warfarin sits in the middle at 2.4. If you’re older, have kidney issues, or are small in frame, apixaban is often the safest pick.
What About Gastrointestinal Bleeding?
Stomach and intestinal bleeding are common worries with blood thinners. DOACs, especially rivaroxaban and dabigatran, carry a slightly higher risk here than apixaban. One 2024 study showed rivaroxaban had a 1.35 times higher chance of GI bleeding compared to apixaban. If you’ve had ulcers or stomach issues before, your doctor might avoid rivaroxaban and pick apixaban or edoxaban instead.
Warfarin doesn’t have a clear edge here. In fact, when combined with NSAIDs like ibuprofen or naproxen, warfarin’s GI bleeding risk spikes. But DOACs aren’t safe with NSAIDs either-the FDA added a warning in 2024: using NSAIDs with DOACs increases GI bleeding risk by more than twice. So no matter which drug you’re on, avoid daily painkillers unless your doctor says it’s okay.
Reversing the Effects: What Happens in an Emergency?
If you fall and hit your head, or have a major surgery, you need to reverse the blood thinner fast. Warfarin has two reliable reversal tools: vitamin K (takes hours to days) and prothrombin complex concentrate (PCC, works in minutes). It’s not perfect, but it’s been used for decades.
DOACs have targeted antidotes-but only for some. Idarucizumab reverses dabigatran. Andexanet alfa reverses apixaban, rivaroxaban, and edoxaban. These drugs are expensive and not always available in small hospitals. But they work quickly, often within minutes.
The big win? DOACs naturally wear off faster. If you miss a dose or need emergency surgery, the drug leaves your system in 12-24 hours. Warfarin can stick around for days. That’s why DOACs are preferred for patients who need surgery or have unpredictable schedules.
Monitoring and Lifestyle: The Hidden Burden
Warfarin isn’t just dangerous-it’s exhausting. You need weekly or monthly INR checks. Your diet matters. Eating a big plate of spinach, kale, or broccoli can drop your INR. A week of fast food or alcohol can spike it. One patient on a support forum said, “My INR dropped from 2.5 to 1.8 after eating spinach. I had to get a new dose in 48 hours.”
DOACs? No diet changes. No weekly blood draws. You take your pill, and that’s it. A 2023 survey of over 1,200 patients found 78% of DOAC users said their quality of life improved. Only 42% of warfarin users felt the same.
And adherence? People stick with DOACs longer. A 2022 analysis showed 28% of warfarin users quit within a year because of the hassle. Only 18% of DOAC users stopped. It’s not just about safety-it’s about being able to live normally.
Who Still Needs Warfarin?
DOACs aren’t the answer for everyone. If you have a mechanical heart valve, DOACs are dangerous. The FDA says they’re not approved for this use. Warfarin is still the only option.
Same goes for antiphospholipid syndrome-a rare autoimmune condition that causes repeated clots. A 2019 trial showed people with this condition had nearly three times more clots on DOACs than on warfarin. So doctors still stick with warfarin here.
Severe kidney disease? That’s another exception. If your kidneys are failing (CrCl below 15-30 mL/min), most DOACs can’t be used safely. Warfarin doesn’t rely on kidneys to clear itself, so it’s often the only choice.
Cost: The Elephant in the Room
Warfarin costs $4 to $10 a month. DOACs? $450 to $600 without insurance. That’s a huge gap.
But here’s the twist: most people with Medicare Part D or private insurance pay $30-$100 a month for DOACs. And when you add up the cost of all those INR tests, doctor visits, hospital stays for bleeding, and emergency reversal treatments, warfarin isn’t always cheaper.
A 2024 study found DOACs become cost-effective after just 13 INR tests a year. If you’re getting tested monthly, you’ve already crossed that line. For many, the real cost isn’t the pill-it’s the time, stress, and risk of complications.
What’s the Best Choice for You?
There’s no one-size-fits-all answer. But here’s what most experts agree on:
- If you have atrial fibrillation and no mechanical valve: DOACs are first-line. Apixaban is often the top pick for safety.
- If you’re over 80, small, or have a history of bleeding: Apixaban is the safest DOAC.
- If you’ve had stomach ulcers: Avoid rivaroxaban. Pick apixaban or edoxaban.
- If you have a mechanical heart valve or antiphospholipid syndrome: Stick with warfarin.
- If you can’t afford DOACs and have good access to INR testing: Warfarin can still work well-if you’re consistent.
Doctors now use a simple 5-point score to help decide: age over 75, kidney problems, past bleeding, taking aspirin or NSAIDs, being female. If you score 3 or more, apixaban is usually the best choice.
What’s Changing in 2025 and Beyond?
Generic apixaban hits the market in 2026. Rivaroxaban follows in 2027. That could cut DOAC prices by 80%. That’s going to make the choice even easier.
New reversal agents are in testing-like ciraparantag, which could reverse all anticoagulants in one shot. That could be a game-changer for emergencies.
And research is starting to look at personalized dosing based on your genes. In the future, your apixaban dose might be adjusted based on your CYP2C9 and VKORC1 genes-just like warfarin is now. But with DOACs, it’s still early days.
Right now, the data is clear: DOACs are safer, simpler, and better for most people. Warfarin still has its place-but it’s shrinking.
Are DOACs safer than warfarin?
Yes, for most people. DOACs reduce the risk of major bleeding by about 30% compared to warfarin, especially dangerous brain bleeds. Apixaban has the lowest bleeding rate among DOACs. They also don’t require frequent blood tests or dietary restrictions, making them easier to manage safely.
Can I switch from warfarin to a DOAC?
Many people can, but it depends on your condition. If you have atrial fibrillation or a blood clot, switching is often recommended. But if you have a mechanical heart valve, antiphospholipid syndrome, or severe kidney disease, you should stay on warfarin. Always consult your doctor before switching-timing and dosing matter.
What’s the cheapest blood thinner?
Warfarin is the cheapest at $4-$10 per month without insurance. DOACs cost $450-$600 without insurance, but with most insurance plans, your copay is $30-$100. When you factor in the cost of blood tests and hospital visits for warfarin complications, DOACs often become more cost-effective over time.
Do DOACs need blood tests?
No, routine blood tests aren’t needed for DOACs. Unlike warfarin, which requires INR checks every few weeks, DOACs have fixed doses and predictable effects. However, your doctor may check kidney function once or twice a year since DOACs are cleared through the kidneys.
What should I avoid while taking a blood thinner?
Avoid NSAIDs like ibuprofen and naproxen-they double the risk of stomach bleeding with both DOACs and warfarin. Limit alcohol, as it can increase bleeding risk. For warfarin, avoid large changes in vitamin K-rich foods like spinach, kale, and broccoli. For DOACs, diet doesn’t matter, but always check with your doctor before starting any new medication or supplement.
Which DOAC has the fewest side effects?
Apixaban (Eliquis) has the lowest risk of major bleeding among DOACs and is often recommended for older adults, people with low body weight, and those with a history of falls or bleeding. It’s also the most studied in real-world populations and has the best safety profile overall.





15 Comments
Just switched from warfarin to apixaban last year and my life’s changed. No more weekly blood draws, no more stressing over spinach salads, and I actually sleep better knowing I won’t bleed out from a tiny fall. Honestly? Worth every penny.
Apixaban’s the safest. Period.
Yessss! 🙌 I’ve been on rivaroxaban for 2 years and honestly? I forget I’m even on a blood thinner. No tests, no fuss. My grandma’s on warfarin and she’s got a whole spreadsheet for her kale intake 😅
Let’s not romanticize DOACs as some kind of medical utopia. The illusion of convenience masks a deeper structural problem: we’ve outsourced vigilance to pharmaceutical corporations. Warfarin demands engagement - and isn’t that, in a way, a form of bodily sovereignty? We’ve traded autonomy for ease, and now we’re surprised when the antidotes cost more than our mortgages.
And let’s not pretend generics will solve anything. The real issue is a healthcare system that commodifies survival.
My uncle in Vancouver’s on warfarin because his kidneys are shot and he can’t afford DOACs even with insurance. It’s not just about what’s safer - it’s about what’s accessible. We need better pricing policies, not just better pills.
My doc pushed me toward apixaban after I had a minor GI bleed on warfarin. Best decision ever. I still eat my greens and drink wine - no guilt. Honestly, if you can get it, just go apixaban. It’s like the Tesla of blood thinners.
It’s wild how much this topic matters. I’ve watched my mom go from weekly finger pricks to a simple daily pill. She went from being anxious about every bruise to hiking again. It’s not just clinical data - it’s about dignity. DOACs don’t just prevent clots, they let people live again.
And yeah, the cost is brutal if you’re uninsured, but the system needs to fix that, not make people feel guilty for wanting safety.
Been on eliquis since 2021 and never looked back. My last INR was 3.2 and I cried because I was so tired of it. Now I just take my pill and go to work. No one even knows I’m on a blood thinner. That’s freedom.
While the data suggests DOACs reduce major bleeding, the studies are heavily skewed toward low-risk populations. Real-world outcomes in polypharmacy elderly patients with multiple comorbidities show significantly higher rates of GI events - particularly with dabigatran. The marketing narrative ignores the complexity of aging physiology. We’re not just treating atrial fibrillation - we’re managing frailty, renal decline, and drug interactions. Apixaban is better, yes - but not universally optimal.
Just wanna say - if you’re over 70 and have had a fall before, apixaban is your BFF. I’m 78, 110 lbs, and my doc said ‘if you’re gonna be on something, let it be this one.’ I don’t even think about it anymore. And honestly? That’s the gift. Not the drug. The peace.
Also - NSAIDs are the silent killer here. I used to take ibuprofen for my knees. Now I use heat packs. Small change. Big difference.
Love that this thread is so practical. My mate in Dublin switched last year and now he’s traveling to Portugal without stressing about bleeding risks. Warfarin was a prison. DOACs? Freedom with a prescription.
Thank you for sharing such a thoughtful, evidence-based breakdown. As a nurse who’s managed dozens of anticoagulated patients, I can confirm: the quality-of-life difference is profound. DOACs empower patients. Warfarin often disempowers. And while cost is a barrier, the long-term savings in ER visits and hospitalizations are undeniable. 💪❤️
If you’re thinking about switching - do it. But don’t just trust the internet. Talk to your hematologist. Get your kidney numbers checked. Apixaban isn’t magic - it’s medicine. And medicine needs context.
Also - if you’re on DOACs and your doctor says ‘no tests needed,’ ask them to check your CrCl every 6 months anyway. Kidneys change. So should your plan.
From a pharmacokinetic standpoint, DOACs offer superior target specificity and reduced interpatient variability due to minimal CYP450 metabolism compared to warfarin’s VKORC1/CYP2C9 polymorphism dependence. However, renal clearance remains a critical confounder - particularly in the elderly, where eGFR decline is often underrecognized. The 2024 AHA guidelines now recommend routine renal monitoring for all DOAC users, regardless of baseline function.
That’s exactly what my doctor said - check kidney function yearly. I didn’t realize how much that mattered. Thanks for the reminder. I’ll schedule mine next week.