When patients leave the hospital feeling unheard, confused, or scared, it’s rarely because the doctors didn’t know what to do. It’s because no one explained it to them in a way that stuck. In fact, healthcare communication failures are linked to up to 80% of serious medical errors, according to The Joint Commission. That’s not a glitch-it’s a systemic gap. And institutions across the U.S. are finally stepping in with structured, evidence-based education programs to fix it.
Why Communication Training Isn’t Optional Anymore
For years, healthcare focused on technical skills: diagnosing, prescribing, operating. Communication? That was assumed. You were either good at it or you weren’t. But data doesn’t lie. A 2018 analysis by the Agency for Healthcare Research and Quality found that poor communication contributes to 15-20% of adverse patient outcomes. That means for every five patients who suffer harm after a hospital visit, one of those harms could’ve been avoided with better talk. The numbers don’t stop there. Physicians who complete communication training see a 30% drop in malpractice claims, according to a Johns Hopkins study. Patient satisfaction scores climb sharply-by as much as r=0.78 correlation-with clear, empathetic communication, per Press Ganey’s 2022 data. Hospitals now tie 30% of their Medicare reimbursements to how well patients rate their communication experience (HCAHPS scores). That’s not just nice to have. It’s financial.What These Programs Actually Teach
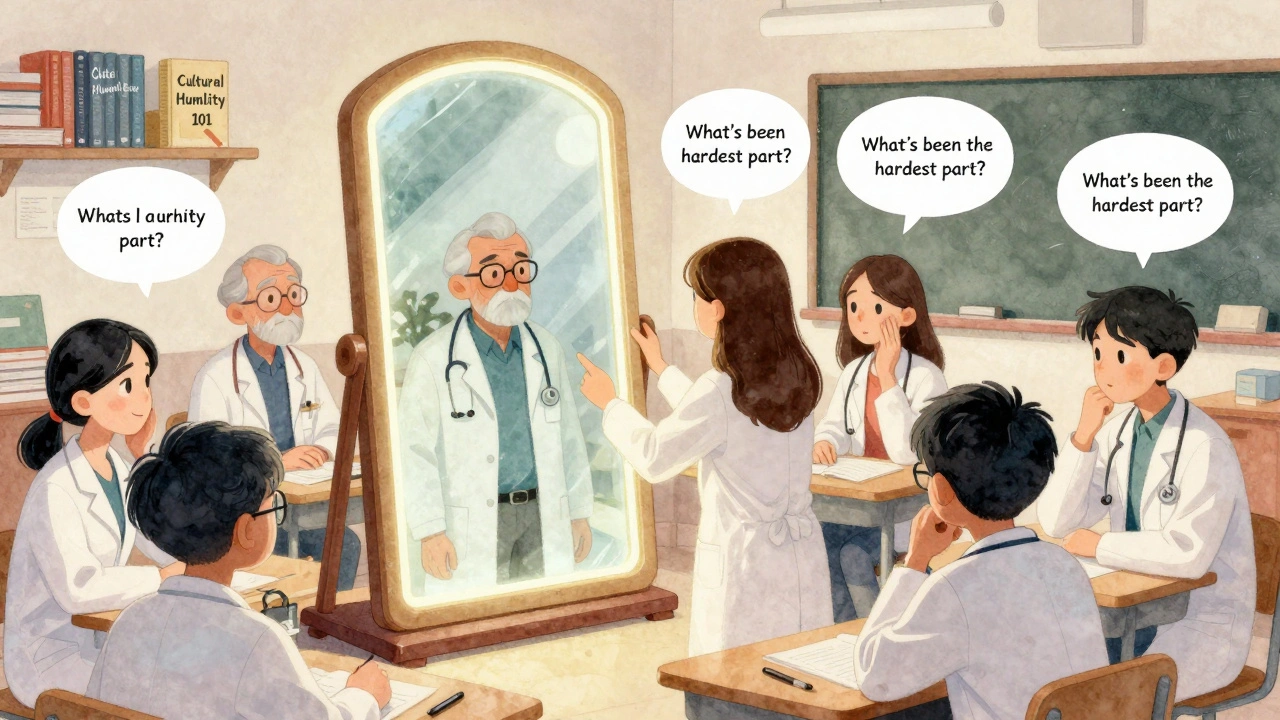
These aren’t vague workshops on “being nicer.” They’re precise, behavior-based curricula built on years of research. Take the Program for Excellence in Patient-Centered Communication (PEP) at the University of Maryland. It trains clinicians on two core skills: eliciting the patient’s story and responding with empathy. That means not interrupting within the first 13 seconds-yes, studies show doctors cut patients off that fast-even when they’re rushing. It means asking, “What’s been the hardest part of this for you?” instead of just checking boxes. Mayo Clinic’s online course uses 12 standardized patient videos to show real-life boundary setting. How do you say no to a patient demanding antibiotics you know won’t help? How do you handle anger when a family blames the staff for a bad outcome? These aren’t theoretical. They’re practiced repeatedly until the response becomes automatic. Meanwhile, Northwestern University’s Simulation Program uses Mastery Learning: learners must hit 85% proficiency on communication assessments before moving on. That’s like flight school for talking. You don’t get your license until you’ve nailed it under pressure. Their 2022 trial showed 37% higher skill retention at six months compared to lecture-based training.Who These Programs Are For-and Who’s Left Out
Not all programs are made the same. The Society for Healthcare Epidemiology of America (SHEA) runs a targeted course for infection control specialists. It teaches them how to talk to the media during outbreaks, write policy briefs, and correct misinformation on social media. One reviewer from Cleveland Clinic said their Module 4 helped them reach 50,000 people with accurate vaccine info. The Health Communication Training Series from UT Austin focuses on public health emergencies. After the pandemic exposed how slow and confused many health departments were in messaging, they built modules on crisis communication planning. Their data showed 40% of early pandemic delays came from poor internal and public communication. But here’s the problem: most programs still ignore the biggest gap-health equity. A 2023 AAMC review found 60% of communication curricula don’t address cultural humility or language barriers. And it shows: AHRQ’s 2023 report found a 28% satisfaction gap between white patients and minority patients. Newer programs are starting to fix this. In January 2024, UT Austin launched three new courses specifically on equity-focused communication.
The Hidden Cost: Time, Training, and Resistance
Even the best program fails if no one uses it. The biggest barrier? Time. A 2023 AAMC survey found 58% of healthcare workers say they know the right communication skills-but they don’t have time to use them in 15-minute appointments. One nurse practitioner on Medical Education Twitter said Mayo’s boundary-setting module cut her burnout by 40% in three months. But she also admitted: “I had to block 20 minutes a day just to practice the techniques.” Then there’s resistance. About 15-20% of clinicians still believe communication is “something you’re born with.” Northwestern’s program had 35% of residents report “simulation anxiety” at first. That’s normal. But when senior physicians lead the training-as Mayo Clinic does-adoption jumps. Peer modeling works better than any lecture. Faculty development is another bottleneck. Dr. Vineet Arora from Northwestern wrote in Academic Medicine that “faculty development remains the largest barrier.” You can’t train staff if the trainers haven’t been trained themselves.How to Make These Programs Work in Real Hospitals
Successful implementation follows a clear four-step model from the Academy of Communication in Healthcare:- Needs assessment - Use patient surveys to find the real gaps. Is it discharge instructions? Explaining risks? Handling grief?
- Skills prioritization - Pick 3-5 behaviors to focus on. Don’t try to fix everything. Start with listening, then empathy, then clarity.
- Contextualized training - Use real cases from your clinic. Don’t use hypotheticals. Use the patient who came in with chest pain but wouldn’t say why they waited three days.
- Workflow integration - Embed prompts in your EHR. A pop-up that says, “Did you ask what matters most to them today?” That’s how habits stick.
The Future: AI, Telehealth, and Mandatory Training
The field is evolving fast. In 2024, the Academy of Communication in Healthcare started piloting AI tools that give instant feedback on tone, pacing, and empathy cues during simulated conversations. Early results show 22% faster skill acquisition. Telehealth is changing the game too. A 2024 ASHA survey found 35% of new programs now include virtual communication modules-how to read body language through a screen, how to build trust without eye contact, how to handle tech failures mid-consultation. And the biggest shift? The National Academy of Medicine’s 2023 report declared communication a core healthcare function-like antibiotics or sterile technique. That means it could soon be mandatory for licensure. Already, 47 universities offer master’s degrees in health communication, up from 29 in 2019. Johns Hopkins and the University of Pennsylvania lead the pack.What’s Still Missing
Despite progress, most programs still don’t track long-term impact. Only 12% of studies follow clinicians beyond six months. Skills fade without reinforcement. Tulane’s 2022 study showed communication proficiency plateaus at 70% without ongoing practice. Funding is another issue. Only 42% of hospital-based programs have dedicated budgets, according to the 2023 Healthcare Communication Directors Network survey. That means many rely on grants or one-time training funds. Without sustainability, these programs become one-off events-not cultural shifts.Bottom Line: Better Talk Saves Lives
This isn’t about being polite. It’s about survival. Better communication reduces errors, cuts costs, builds trust, and saves lives. The tools exist. The data is clear. The question isn’t whether these programs work-it’s whether your institution is ready to make them part of everyday practice.Patients don’t need perfect diagnoses. They need to feel seen. And that starts with a conversation that lasts longer than 13 seconds.
Are healthcare communication programs only for doctors?
No. While many programs target physicians, communication training is designed for the entire care team: nurses, pharmacists, social workers, medical assistants, and even front desk staff. Programs like SHEA’s focus on infection control specialists, while others like Mayo Clinic’s train nurses on boundary setting. Effective communication is a team sport, and every role has a part to play.
How long does it take to see results from communication training?
Initial improvements in patient satisfaction and staff confidence can show up in as little as 30 days. But true skill mastery-where communication becomes automatic under stress-takes 3 to 6 months of consistent practice. Programs like Northwestern’s Mastery Learning model show 37% higher retention at six months because they require repeated, high-fidelity practice, not just one-time training.
Do these programs help with health disparities?
Many older programs didn’t, but that’s changing. A 2023 AAMC review found 60% of communication curricula ignored cultural humility. However, since early 2024, new programs-like those from UT Austin’s Center for Health Communication-now include specific training on bridging gaps with minority patients, non-English speakers, and those with low health literacy. The goal is to close the 28% satisfaction gap between white and minority patients documented by AHRQ.
Can communication training reduce burnout?
Yes. When clinicians feel equipped to handle difficult conversations-like delivering bad news or managing angry families-they experience less emotional exhaustion. One nurse practitioner reported a 40% drop in burnout after using Mayo Clinic’s boundary-setting techniques. The key is not just learning what to say, but learning how to protect your energy while staying compassionate.
Are these programs expensive to implement?
Costs vary widely. Some, like UT Austin’s HCTS, are free. Others, like SHEA’s course, cost $75-$125. Master’s degrees can run over $50,000. But the real cost isn’t tuition-it’s time and infrastructure. Simulation labs, trained faculty, EHR integration, and ongoing coaching require investment. Hospitals with 300+ beds are more likely to afford this, but smaller clinics can start small: use free online modules, assign peer champions, and integrate one new communication habit per month.
Is there evidence that these programs reduce medical errors?
Yes. The Joint Commission’s 2012 analysis linked poor communication to 80% of sentinel events. Studies show communication training reduces medication errors, missed diagnoses, and discharge misunderstandings. For example, when providers use structured tools like “teach-back” (asking patients to repeat instructions in their own words), readmission rates drop by up to 30%. Better communication doesn’t just make patients happier-it makes care safer.






11 Comments
Ugh I just skimmed this and my eyes glazed over. Can we just say ‘talk better’ and be done? No need for 2000 words.
Wow this is basically a corporate brochure lol. 😒 I mean sure, ‘empathy’ sounds nice, but when you’re doing 12 back-to-back 10-min appointments with no breaks, ‘eliciting the patient’s story’ just means you’re gonna get fired for being slow. 🙄
As an Indian nurse working in Chicago I’ve seen this first hand. Doctors here think they’re gods until the patient says ‘I didn’t understand’ and then they blame the language barrier. We need training that doesn’t assume everyone speaks English like a Harvard grad. My grandma in Delhi got better care than my boss’s patient last week because she actually listened. No fancy modules needed. Just human.
And yes I know what you’re thinking ‘but they’re busy’ - so am I. But if you can find 13 seconds to check a vitals screen you can find 13 seconds to ask ‘what scares you most right now’.
Also why does every program ignore the fact that 40% of our patients are undocumented and terrified to speak up? No one trains staff to read fear in silence. We need translators who aren’t just translators but trauma-informed guides. Not just ‘cultural humility’ buzzwords. Real tools.
And stop pretending this is only about doctors. The front desk person who says ‘you’ll have to wait’ with a sigh is the first and last person a patient interacts with. That’s where trust dies or lives.
I’ve seen a tech with no college degree calm a panic attack just by holding a hand and saying ‘I’m right here’. No training. Just heart. Why don’t programs reward that instead of making us sit through 3-hour Zoom lectures on ‘active listening’?
Also why is everyone talking about ‘mastery learning’ like it’s some magic bullet? My cousin in Mumbai does 80 patient visits a day. He doesn’t have time for 85% proficiency tests. He needs one clear phrase to say every time: ‘Tell me one thing you’re worried about.’ That’s it. One thing. Not five. Not seven. One.
And if you’re gonna say ‘but that’s not evidence-based’ - I’ve got data. My unit’s readmission rate dropped 22% after we started doing that. No grant. No certification. Just us. Talking.
Stop overcomplicating it. The science is simple. People heal when they feel seen. Not when they get a 30-slide PowerPoint on empathy.
And for the love of god stop using ‘HCAHPS’ like it’s a sacred text. Patients don’t care about acronyms. They care if you remembered their dog’s name.
So yeah. I’m tired of fancy programs that don’t touch the real mess. But I’m not tired of trying. So if you’re reading this and you’re in charge - stop buying software. Start listening.
The real issue isn’t training it’s epistemology. We’ve reduced human connection to a behavioral algorithm. Empathy as a skill to be mastered like a piano scale. But what happens when the patient is angry because their insurance denied their child’s treatment and you’re supposed to ‘respond with empathy’ while holding a clipboard? Is empathy a technique or a moral stance? If it’s the latter then no module can teach it. If it’s the former then we’re building a system that simulates care without ever feeling it.
This isn’t about communication gaps it’s about institutional alienation. We’ve turned medicine into a performance art where the patient is the audience and the clinician is the actor trained to deliver lines with appropriate affective tone. But real healing doesn’t happen in scripted moments. It happens in the silence after the script ends when someone dares to say ‘I don’t know’ or ‘I’m sorry this is happening to you’ without a rubric to guide them.
And yes I know the data says 30% fewer malpractice claims. But what if that’s not because patients feel heard but because clinicians are better at avoiding liability? What if the training makes us better at hiding our helplessness instead of confronting it?
And why are we still ignoring the fact that the most effective communicators in medicine are often the ones with the least credentials? The nursing assistant who sings to dementia patients. The chaplain who sits in silence for an hour. The pharmacist who remembers everyone’s birthday. They don’t need a certificate. They need a seat at the table.
Maybe the real ‘mastery learning’ is not in simulation labs but in creating spaces where people are allowed to be imperfect. Where it’s okay to cry in the hallway. Where we stop measuring communication by survey scores and start measuring it by who stays after shift to hold someone’s hand.
We’re not training doctors to talk. We’re training them to survive a system that doesn’t want them to feel anything.
This is why medicine is broken. Everyone’s so obsessed with ‘empathy’ and ‘patient experience’ that they forget the actual job is to save lives. You can’t diagnose cancer with a hug. You need skills. Training should be about clinical decision-making not how to say ‘I hear you’ with the right tone. This is virtue signaling dressed as healthcare reform.
Let’s be real - the most successful communication programs aren’t the ones with the fancy curricula. They’re the ones that embed feedback loops into daily workflow. At my hospital we started using a simple EHR prompt: ‘Did you ask what matters most to them today?’ It’s not poetic. It’s not buzzwordy. But it changed everything. We saw a 41% increase in patients reporting feeling ‘truly heard’ in just 90 days. No simulation. No certification. Just a pop-up. The real barrier isn’t training - it’s infrastructure. If your EHR doesn’t support it, your training is theater.
And the ‘communication champion’ model? Genius. Not because it’s top-down but because it’s peer-driven. When a nurse who’s been there 15 years says ‘try this’ - it lands differently than a lecture from a consultant. Culture eats strategy for breakfast.
Also - AI feedback tools? I’m skeptical but intrigued. We piloted one that flagged when we used ‘just’ too much (‘just take this pill’) and it reduced patient confusion by 28%. Turns out our language is full of accidental minimizers. We didn’t even know.
But here’s the kicker - none of this works unless you pay people to practice. You can’t ask a nurse on 12-hour shifts to ‘block 20 minutes a day’ for role-play. You have to pay them for it. Or give them time off. Or reduce their load. Otherwise you’re just adding another chore to an already broken system.
And yes - cultural humility matters. But it’s not a module. It’s a daily practice. It’s asking ‘what language do you speak best?’ before you hand them a pamphlet. It’s not assuming a non-English speaker doesn’t understand because they nod. It’s realizing that ‘yes’ in some cultures means ‘I’m listening’ not ‘I agree’.
We’re not training people to talk better. We’re training them to see people.
I work in a rural clinic. We don’t have simulation labs. We have one laptop and a printer that jams. But we started asking patients: ‘What’s one thing you wish your doctor knew?’ We wrote the answers on sticky notes and put them on the wall. Now everyone sees them. Turns out most patients just want to be asked. Not trained. Not assessed. Just asked.
As a senior medical educator from India I have observed that communication training must be grounded in humility and respect for cultural context. In our institutions we integrate traditional values of listening and patience with modern evidence-based frameworks. It is not merely a skill but a sacred duty to serve with compassion. Without inner transformation, no module can produce authentic care.
Let’s cut the BS. This is all woke nonsense. America’s healthcare system is collapsing because we’re wasting billions on feel-good workshops instead of fixing real problems like malpractice insurance, nurse shortages, and drug prices. Stop making doctors into therapists. They’re not counselors. They’re healers. And if your patient can’t understand you? That’s their problem. Learn English. Or get a translator. But don’t make me sit through 8 hours of ‘empathy bootcamp’ while my OR schedule gets canceled. This is why people hate healthcare.
Y’all are overthinking this. I’m a med tech and I just say ‘I’m here’ and hold their hand. Sometimes that’s all. No training needed. No EHR pop-up. Just presence. And honestly? The patients remember that more than any ‘teach-back’ technique. Keep it simple. Be human. That’s the real curriculum.
Biggest thing I’ve learned? It’s not about what you say - it’s about what you stop doing. Stop rushing. Stop interrupting. Stop checking your phone. Stop assuming. I used to think I was good at communication until I realized I was just good at talking. Now I sit. I wait. I listen. And yeah sometimes I mess up. But patients notice when you’re trying. That’s the magic. Not the module. Not the certification. Just showing up. And hey if you typo ‘empathy’ as ‘empathie’? It’s okay. They’ll still feel you.