Warfarin: What It Is, How It Works, and What You Need to Know
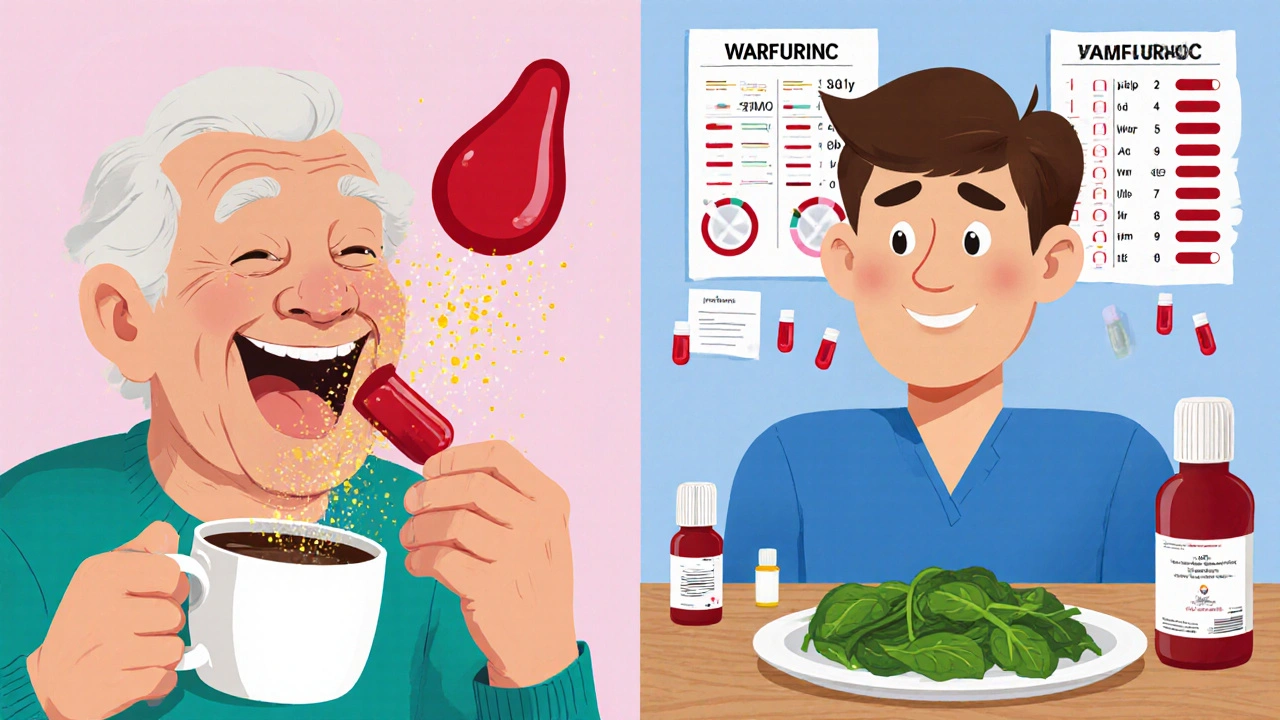
When your doctor prescribes warfarin, a blood-thinning medication used to prevent dangerous clots in the heart, legs, or lungs. Also known as Coumadin, it’s one of the most prescribed anticoagulants in the world — but it’s not simple to use. Unlike newer blood thinners that come with fixed doses, warfarin demands attention. Your body reacts differently to it than anyone else’s. One person might need 5 mg a day, another 10 mg — and even then, it can shift without warning.
What makes warfarin tricky is how much it depends on INR monitoring, a blood test that measures how long it takes your blood to clot. Too low, and you risk clots that could cause a stroke or pulmonary embolism. Too high, and you could bleed internally from a minor bump or cut. That’s why people on warfarin get regular blood draws — sometimes every week, sometimes every month. It’s not just a pill you take and forget. It’s a balancing act.
And then there’s drug interactions, how other medications, supplements, or even food change how warfarin works in your body. Antibiotics, painkillers, herbal teas like St. John’s wort, and even a big bowl of spinach can throw your INR off. It’s not just about what you take — it’s about what you eat, what you stop taking, and even how much alcohol you drink. That’s why people on warfarin often end up with thick binders full of notes, or apps that track every pill, meal, and test result.
Warfarin isn’t going away. Even with newer options like apixaban or rivaroxaban, many people still rely on it — because it’s cheap, it’s been around for decades, and doctors know how to manage it. But that doesn’t mean it’s easy. It’s a medication that rewards consistency: same time every day, same diet, same habits. Skip a dose? Eat a lot of kale? Start a new antibiotic? Your INR could swing overnight.
If you’re on warfarin, you’re not alone. Millions of people take it every day — for atrial fibrillation, after a heart valve replacement, after deep vein thrombosis, or because of a history of clots. But the stories you hear aren’t always about success. Some people get scared of bruising. Others panic when their INR is high. A few end up in the ER because they didn’t realize their cold medicine could be dangerous. The good news? With the right knowledge, most of those risks can be avoided.
Below, you’ll find real, practical guides that break down what warfarin really means in daily life — from how it interacts with other drugs like hydrochlorothiazide or aspirin, to why some people need ECG checks when switching therapies, and how to avoid common mistakes that lead to hospital visits. These aren’t theoretical articles. They’re written by people who’ve lived with this, or who help others manage it every day. Whether you’re just starting warfarin or you’ve been on it for years, there’s something here that will make your life safer and simpler.
Using Food Diaries on Warfarin: Tracking Vitamin K for Safety
Tracking vitamin K with a food diary is essential for warfarin patients to maintain stable INR levels and avoid dangerous bleeding or clotting risks. Consistency in diet beats restriction.
Keep ReadingDirect Oral Anticoagulants vs Warfarin: Side Effect Comparison
DOACs like apixaban and rivaroxaban offer fewer bleeding risks and no need for blood tests compared to warfarin, making them the preferred choice for most patients. Learn who still needs warfarin and how to choose the safest option.
Keep ReadingGinkgo Biloba and Blood Thinner Interactions: What You Need to Know
Ginkgo Biloba may increase bleeding risk when taken with blood thinners like warfarin, aspirin, or clopidogrel. Learn what the science says, which combinations are dangerous, and what to do if you're already taking both.
Keep Reading