Thiazide Diuretic: What It Is and Why It Matters
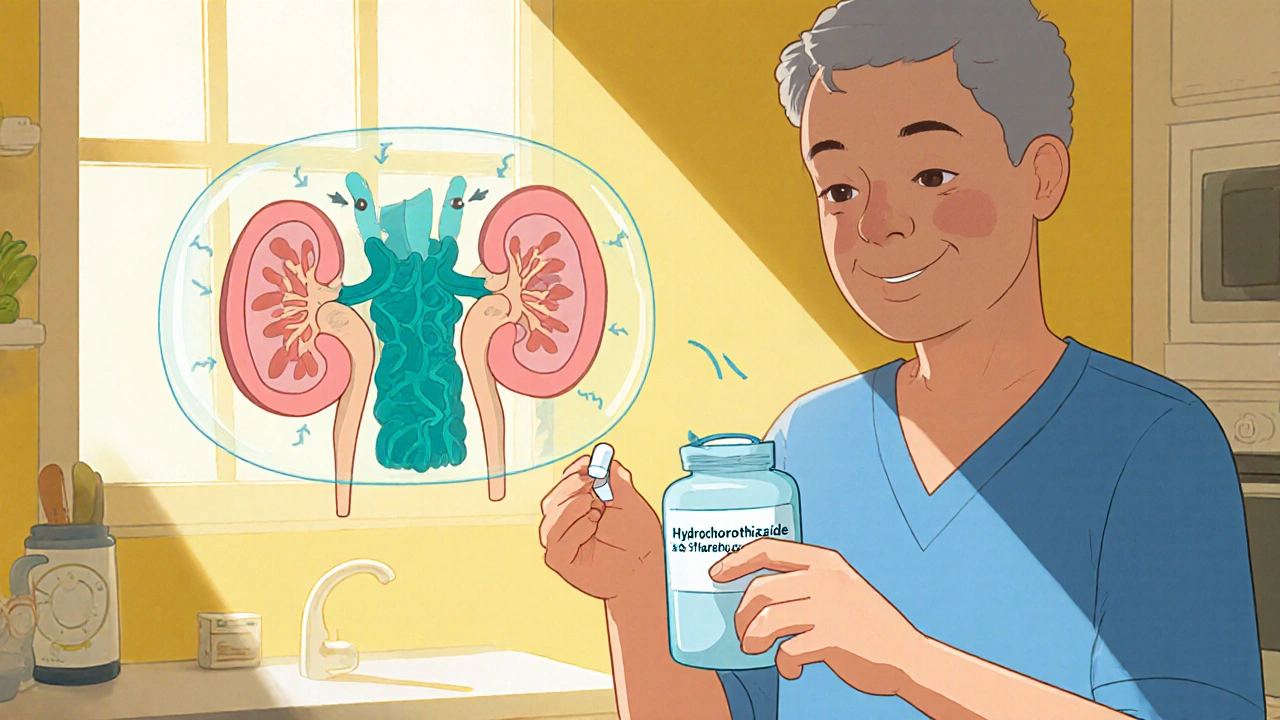
When dealing with thiazide diuretic, a class of pills that help the kidneys get rid of extra salt and water. Also known as thiazide, it’s often prescribed to manage high blood pressure and reduce swelling. If you’re searching for thiazide diuretic info, you’ve come to the right place. Below we break down how it works, the main drugs in the family, and where it fits into broader medication choices.
Thiazide diuretics lower blood pressure by increasing sodium excretion, which pulls water out of the bloodstream – a classic subject‑predicate‑object relationship: thiazide diuretics promote sodium loss, which reduces plasma volume, which decreases arterial pressure. This mechanism also explains why they can affect electrolyte balance; potassium often drops, so doctors keep an eye on labs. The same principle links thiazides to kidney function, because the kidneys are the organ that actually does the filtering.
Key Points About Thiazide Diuretics
One of the most widely used examples is hydrochlorothiazide, a short‑acting thiazide that’s cheap and effective. Another variant, chlorthalidone, offers a longer duration of action, is favored for chronic control. Both share the core attribute of blocking the Na⁺/Cl⁻ transporter in the distal tubule, but chlorthalidone stays in the body longer, giving steadier blood pressure control.
Effective blood pressure control, often combines thiazides with other agents like ACE inhibitors or ARBs because using two different mechanisms can achieve lower targets with fewer side effects. For instance, an ACE inhibitor reduces angiotensin‑II‑driven vasoconstriction while a thiazide cuts fluid volume – together they hit pressure from two angles. This combination principle shows how thiazides interact with a broader medication ecosystem.
Side effects are a real part of the picture. The most common issues are low potassium, higher uric acid (which can trigger gout), and a slight rise in blood sugar. Knowing these risks helps you and your doctor decide on dosing and whether you need a potassium‑sparing partner like spironolactone. Monitoring is simple: regular blood tests for electrolytes and kidney function keep things safe.
When it comes to dosing, hydrochlorothiazide typically starts at 12.5‑25 mg daily, while chlorthalidone may begin at 12.5‑25 mg but is taken every other day or once daily because of its longer half‑life. Adjustments depend on how your blood pressure responds and what side effects appear. For patients with resistant hypertension, adding a thiazide‑type diuretic is often the first step before moving to stronger agents.
The collection of articles below reflects all these angles: drug comparisons, side‑effect management, and practical tips for using thiazides in real‑world scenarios. Whether you’re looking for a quick rundown of hydrochlorothiazide versus chlorthalidone, or you need deeper insight on combining thiazides with other heart medicines, you’ll find concise, evidence‑based guidance that fits everyday decisions. Dive in to see how each piece fits into the bigger picture of blood pressure care.
Hydrochlorothiazide vs Alternatives: A Practical Comparison
A clear, side‑by‑side look at Hydrochlorothiazide and its common alternatives, covering how they work, dosing, effectiveness, and key safety points for hypertension management.
Keep Reading