Hypertension Medication Selection Tool
This tool helps you identify which hypertension medication might be most suitable for your situation based on your health conditions and personal preferences.
Medical Conditions
Lifestyle Factors
When it comes to managing hypertension, Hydrochlorothiazide is one of the most prescribed thiazide diuretics, but it’s not the only option on the shelf. Below you’ll find a straight‑forward comparison of this drug with the most common alternatives, so you can see which one fits your health goals and lifestyle.
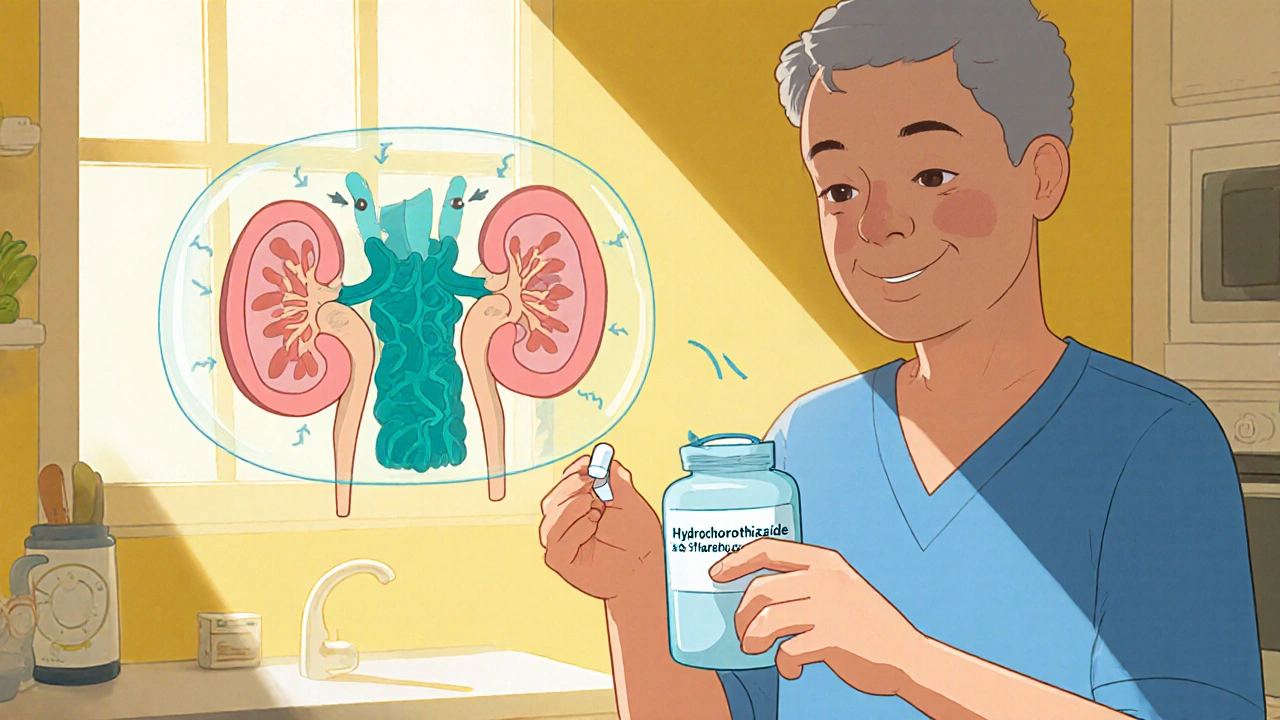
What is Hydrochlorothiazide?
Hydrochlorothiazide is a thiazide‑type diuretic that helps the kidneys eliminate excess sodium and water, lowering blood volume and, consequently, blood pressure. It was first approved in the 1950s and today appears in many combination pills for hypertension and edema. The drug’s typical dose ranges from 12.5 mg to 50 mg once daily, and it works best when taken in the morning to avoid nighttime bathroom trips.
How Hydrochlorothiazide Works
The active ingredient blocks the sodium‑chloride cotransporter in the distal convoluted tubule of the nephron. By reducing sodium reabsorption, more water follows, leading to a modest drop in blood volume. This mechanism also triggers a slight decrease in peripheral vascular resistance, which adds to the blood‑pressure‑lowering effect.
Common Alternatives
Below are the most frequently prescribed drugs that doctors consider instead of, or alongside, Hydrochlorothiazide. Each entry includes a quick definition, typical dosing, and a note on what makes it distinct.
-
Chlorthalidone is a long‑acting thiazide‑like diuretic that offers a smoother blood‑pressure curve over 24 hours, often preferred for patients who need tighter control. Typical dose: 12.5‑25 mg once daily.
-
Indapamide combines diuretic action with vasodilatory properties, making it useful for patients with isolated systolic hypertension. Typical dose: 1.5‑2.5 mg once daily.
-
Metolazone is a potent thiazide‑type diuretic that works even when kidney function is reduced, often added in resistant hypertension. Typical dose: 2.5‑10 mg once daily.
-
Spironolactone is a potassium‑sparing diuretic that antagonizes aldosterone; it’s a go‑to for patients with resistant hypertension or heart‑failure‑related fluid overload. Typical dose: 25‑100 mg once daily.
-
Furosemide belongs to the loop‑diuretic class, providing a rapid, powerful diuresis; it’s reserved for severe edema or when thiazides aren’t enough. Typical dose: 20‑80 mg once or twice daily.
-
Lisinopril is an ACE inhibitor that lowers blood pressure by relaxing blood vessels; it’s often paired with diuretics for synergistic effect. Typical dose: 10‑40 mg once daily.
-
Atenolol is a beta‑blocker that reduces heart rate and contractility, useful in patients with high heart‑rate‑driven hypertension. Typical dose: 50‑100 mg once daily.
Side‑by‑Side Comparison Table
| Drug | Class | Typical Dose | Duration of Action | Potency (relative) | Main Side Effects |
|---|---|---|---|---|---|
| Hydrochlorothiazide | Thiazide diuretic | 12.5‑50 mg daily | 6‑12 h | Moderate | Low potassium, ↑ uric acid, mild glucose rise |
| Chlorthalidone | Thiazide‑like diuretic | 12.5‑25 mg daily | >24 h | High | Hypokalemia, hyponatremia, gout flare |
| Indapamide | Thiazide‑like diuretic | 1.5‑2.5 mg daily | 24 h | Moderate‑high | Electrolyte shifts, dizziness |
| Metolazone | Thiazide‑type diuretic | 2.5‑10 mg daily | 8‑12 h | High (even in CKD) | Severe potassium loss, dehydration |
| Spironolactone | Potassium‑sparing diuretic | 25‑100 mg daily | 24 h | Low‑moderate | Hyperkalemia, gynecomastia |
| Furosemide | Loop diuretic | 20‑80 mg 1‑2×/day | 2‑6 h | Very high | OtO, hypokalemia, ototoxicity |
| Lisinopril | ACE inhibitor | 10‑40 mg daily | 24 h | Variable | Cough, angioedema, hyperkalemia |
| Atenolol | Beta‑blocker | 50‑100 mg daily | 12‑24 h | Low‑moderate | Bradycardia, fatigue, cold extremities |
How to Pick the Right Drug for You
Choosing a blood‑pressure pill isn’t a one‑size‑fits‑all decision. Here are the key factors you should weigh:
- Potency and duration. If you need a steady 24‑hour effect, Chlorthalidone or Indapamide might edge out Hydrochlorothiazide.
- Kidney function. Metolazone works better when creatinine clearance drops below 30 mL/min, whereas loop diuretics like Furosemide are the go‑to for severe renal impairment.
- Electrolyte concerns. Patients prone to low potassium may appreciate the potassium‑sparing action of Spironolactone, or they might need a potassium supplement if they stay on a thiazide.
- Cost and formulary coverage. Hydrochlorothiazide is often the cheapest generic, while newer agents like Indapamide can be pricier.
- Other health conditions. Diabetes, gout, or heart failure can shift the balance toward agents that avoid raising uric acid or that provide extra heart‑protective benefits.

Practical Tips for Patients
- Take your diuretic in the morning to reduce nighttime trips to the bathroom.
- Check your blood pressure twice a week for the first month after a switch.
- Ask your doctor for a baseline and follow‑up electrolyte panel (sodium, potassium, magnesium).
- If you notice muscle cramps, dizziness, or sudden weight loss, call your healthcare provider-these can signal excess fluid loss.
- Never stop a medication abruptly without professional advice; a sudden rise in blood pressure can be dangerous.
Frequently Asked Questions
Can I use Hydrochlorothiazide and a loop diuretic together?
Yes, doctors sometimes combine a thiazide with a loop diuretic to tackle resistant hypertension, but they will monitor potassium and kidney function closely.
Why do I get a gout flare when I start a thiazide?
Thiazides reduce the kidney’s ability to excrete uric acid, which can cause a buildup that triggers gout attacks.
Is Spironolactone safe for women who want to become pregnant?
Spironolactone is classified as pregnancy‑category C; doctors usually avoid it in women trying to conceive because of potential hormonal effects.
What’s the biggest advantage of Chlorthalidone over Hydrochlorothiazide?
Chlorthalidone stays active longer, giving steadier blood‑pressure control and often reducing the need for a second medication.
Do ACE inhibitors like Lisinopril work without a diuretic?
They can, especially in mild hypertension, but many guidelines recommend adding a low‑dose diuretic for better long‑term outcomes.






9 Comments
The history of diuretic therapy is riddled with hidden agendas that mainstream medicine prefers to conceal.
The mid‑20th century onward, large pharmaceutical conglomerates have famously promoted hydrochlorothiazide as the cheap, first‑line solution, regardless of individual patient nuances.
This promotion aligns neatly with profit models that thrive on mass prescriptions rather than tailored therapeutics.
By contrast, agents such as chlorthalidone or indapamide, though pharmacologically superior in many respects, receive scant attention because they lack the same market saturation.
The patent landscape further entrenches this bias, as generic hydrochlorothiazide enjoys an unrivaled supply chain that keeps costs low and demand high.
Yet the cost advantage often masks a cascade of downstream complications, including electrolyte disturbances and gout flares, which ultimately burden the healthcare system.
Moreover, the selective reporting of clinical trials amplifies the perception of safety while downplaying the prevalence of hypokalemia.
A critical appraisal of the comparative table reveals that the duration of action for hydrochlorothiazide rarely exceeds twelve hours, necessitating additional dosing in many patients.
In a world where 24‑hour blood pressure control is the gold standard, relying on a short‑acting agent feels like a deliberate compromise.
The alternative thiazide‑like diuretics, for instance chlorthalidone, provide a more stable antihypertensive profile that can reduce the need for polypharmacy.
Patients with chronic kidney disease likewise benefit from agents such as metolazone, whose efficacy persists despite reduced glomerular filtration.
The omission of these nuances in popular guidelines hints at a systematic undervaluation of clinical heterogeneity.
In addition, the potential for drug‑drug interactions involving spironolactone or ACE inhibitors is often glossed over, despite their relevance in resistant hypertension.
A truly patient‑centered approach would involve a thorough assessment of comorbidities, renal function, and electrolyte balance before settling on a one‑size‑fits‑all prescription.
Clinicians should therefore interrogate the economic incentives that shape formulary decisions and advocate for evidence‑based personalization.
Only by exposing these concealed mechanisms can the medical community restore autonomy to therapeutic decision‑making.
The practical tip to take diuretics in the morning is essential for minimizing nocturia and preserving sleep quality.
Monitoring blood pressure twice weekly during a medication switch offers a realistic window to detect efficacy and adverse trends.
Baseline electrolyte panels are a cornerstone of safe diuretic therapy, especially when combining thiazides with potassium‑sparing agents.
Patients should also be aware that gout flares can be precipitated by thiazide‑induced hyperuricemia, warranting proactive management.
Overall, this guide empowers individuals to engage actively with their treatment plan and collaborate with their physicians.
Great breakdown; this will help many patients stay on track!
Life is a series of choices and a pill is just one of them yet we tend to overthink its significance.
The table reminds us that chemistry is indifferent to our anxieties.
Embrace the data and let the numbers guide you.
The comparative matrix exhibits a robust pharmacodynamic stratification but neglects the pharmacokinetic variability inherent to renal clearance fluctuations.
Moreover, the omission of dose‑response curves for each agent undermines the granularity required for precision dosing.
While the side‑effect profile is delineated, the hierarchical weighting of adverse event severity lacks a validated scoring algorithm.
A more rigorous meta‑analytic synthesis could reconcile the heterogeneity across pivotal trials and yield a statistically sound hierarchy.
Consequently, clinicians should approach the presented hierarchy with caution and supplement it with individualized risk‑benefit modeling.
The cold hard numbers stare back like a silent judge and the glass ceiling of generic bias shatters when truth is spoken.
We must tear down the illusion of uniform safety and recognize the hidden torment of electrolyte loss.
Only then can the medical narrative be reborn.
Your exposition sheds light on systemic influences that merit deeper discussion among prescribers.
It is advisable to integrate patient-specific factors such as comorbid gout or renal impairment when selecting a diuretic.
Shared decision‑making, supported by transparent risk communication, can mitigate the impact of commercial bias.
Continued professional education on emerging evidence will further enhance therapeutic precision.
Absolutely, the conversation needs that extra spark of empathy to cut through the corporate fog.
Let’s keep the dialogue alive and guide patients toward choices that truly fit their lives!
Selecting an antihypertensive requires alignment of pharmacologic properties with individual patient profiles.
The table serves as a concise reference for that alignment.