Hydrochlorothiazide – What It Is, How It Works, and What You Need to Know
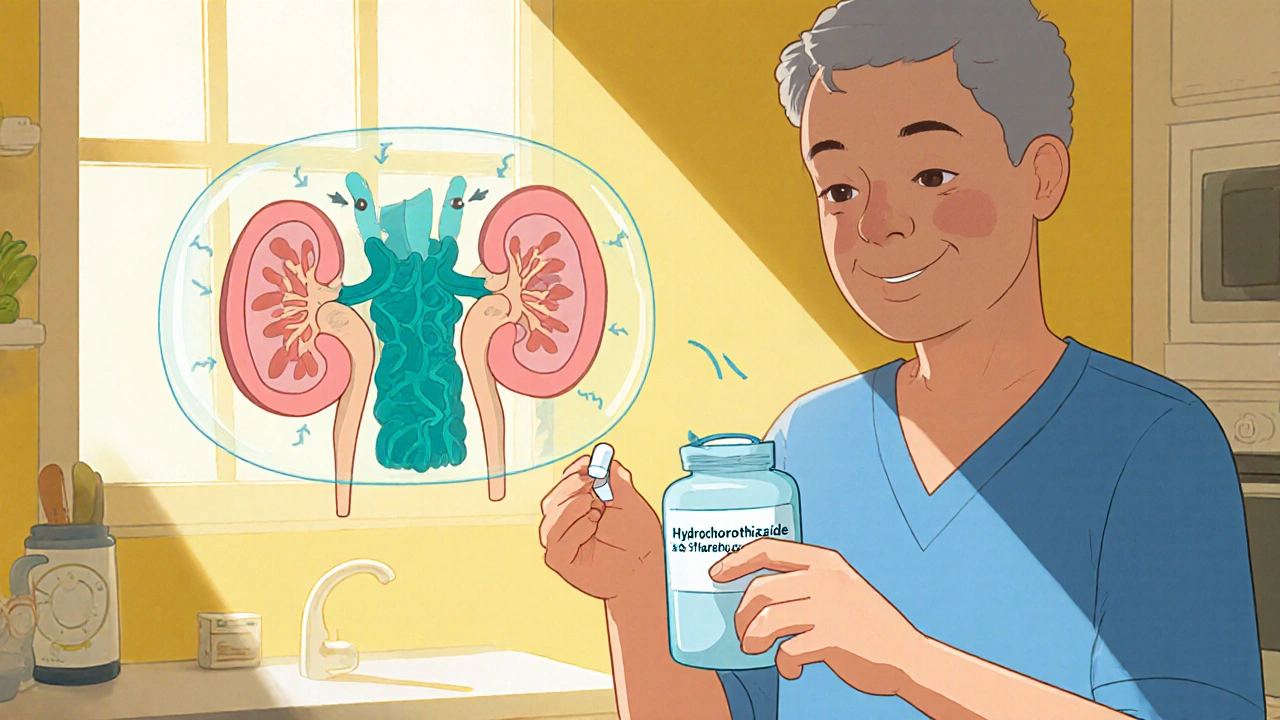
When dealing with Hydrochlorothiazide, a thiazide‑type diuretic used to lower blood pressure and reduce fluid buildup. Also known as HCTZ, it works by prompting the kidneys to excrete more sodium and water, which in turn eases the heart's workload. This simple mechanism makes it a staple in many treatment plans for cardiovascular health.
Hydrochlorothiazide belongs to the broader class of thiazide diuretics, medications that increase urine output by blocking sodium reabsorption in the distal tubule. By reducing plasma volume, thiazides help control hypertension, the chronic elevation of arterial pressure that strains the heart and vessels. They also target edema, abnormal fluid accumulation often seen in heart failure or kidney disease, making swelling less noticeable. In short, Hydrochlorothiazide encompasses fluid regulation, requires kidney function, and influences blood pressure control.
Typical dosing starts low – often 12.5 mg to 25 mg once daily – and can be adjusted based on response and lab results. Doctors may prescribe it alone or pair it with other blood‑pressure pills like ACE inhibitors or calcium‑channel blockers for a stronger effect. The drug is taken in the morning to avoid night‑time bathroom trips, and it works best when you stay hydrated but not overly fluid‑loaded. Adjustments are common for patients with chronic kidney disease, where the kidneys' ability to filter may be reduced.
Side effects are usually mild but worth watching. The most common issue is electrolyte imbalance, especially low potassium (hypokalemia). Symptoms can include muscle cramps, fatigue, or irregular heartbeat. Some people develop higher uric acid levels, which can trigger gout attacks. Less frequent concerns are increased blood sugar, photosensitivity, and rare cases of severe allergic reactions. If you notice sudden weight loss, dizziness, or excessive thirst, it could signal dehydration or a serious electrolyte shift.
Drug interactions matter a lot with Hydrochlorothiazide. NSAIDs (like ibuprofen) can blunt its blood‑pressure‑lowering effect and stress the kidneys. Lithium levels may rise, raising the risk of toxicity. Certain antibiotics, such as ciprofloxacin, can also increase the chance of low potassium. Always tell your healthcare provider about over‑the‑counter medicines or supplements you take, especially potassium‑rich ones or vitamin D, which could affect calcium balance.
Monitoring is straightforward: blood tests for potassium, sodium, creatinine, and uric acid should be done before starting treatment and periodically thereafter. If your potassium dips below 3.5 mmol/L, your doctor might add a potassium‑sparing diuretic or suggest a diet rich in bananas, oranges, and leafy greens. For those with a history of gout, a low‑purine diet and occasional medication adjustments can keep flare‑ups at bay.
Special populations need extra care. Older adults often have reduced kidney function, so a lower starting dose is prudent. Pregnant or nursing women should only use Hydrochlorothiazide if the benefits outweigh potential risks, as it crosses the placenta. Athletes sometimes misuse the drug for rapid weight loss, but this can lead to severe dehydration, cramps, and performance deficits.
Understanding Hydrochlorothiazide helps you make smarter choices about your heart health and fluid balance. Below you’ll find a curated set of articles that dive deeper into related topics—comparisons with other diuretics, tips for managing side effects, and practical guides on combining it with other medications. Keep reading to get the full picture and practical advice you can apply right away.
Hydrochlorothiazide vs Alternatives: A Practical Comparison
A clear, side‑by‑side look at Hydrochlorothiazide and its common alternatives, covering how they work, dosing, effectiveness, and key safety points for hypertension management.
Keep Reading