Blood Pressure Drugs: Your Guide to Choices and Safety
When working with blood pressure drugs, medications that lower arterial pressure to prevent heart attacks, strokes, and kidney damage. Also known as antihypertensives, they are prescribed for anyone diagnosed with high blood pressure or at risk of cardiovascular events. Understanding how they work helps you pick the right regimen and avoid unwanted side effects.
Key Classes You Should Know
First up are ACE inhibitors, drugs that block the enzyme converting angiotensin I to angiotensin II, a powerful vessel‑tightening hormone. Common examples include lisinopril and enalapril, and they often lower blood pressure within a few weeks. Next, beta blockers, medicines that reduce heart rate and contractility by blocking adrenaline receptors. They’re handy when you need both heart‑rate control and pressure reduction. Calcium channel blockers, agents that relax vascular smooth muscle by inhibiting calcium influx, such as amlodipine, are great for people whose pressure spikes at night.
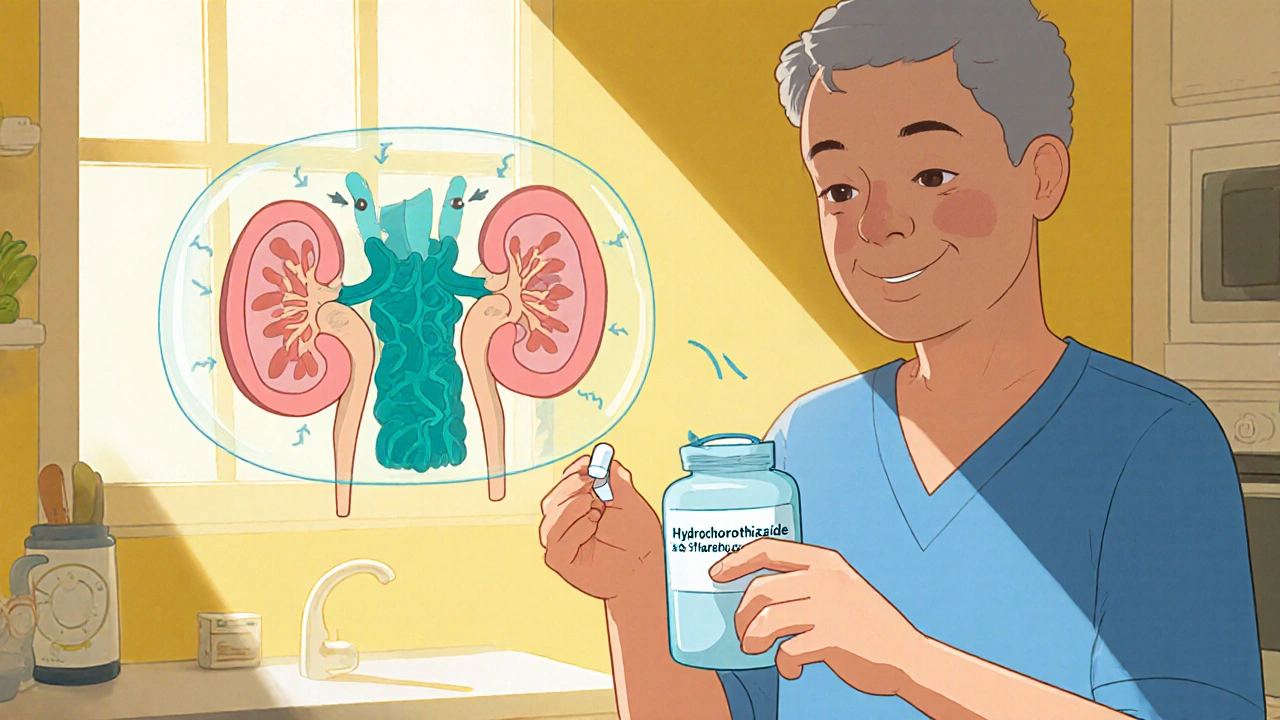
Other important players include diuretics, water‑pills that help the kidneys eliminate excess salt and fluid, easing pressure on blood vessels. Often the first line in treatment, they pair well with the other classes for a multi‑target approach. Together, these groups form a toolbox that clinicians draw from based on age, kidney function, and co‑existing conditions like diabetes.
Knowing the differences matters because blood pressure drugs aren’t one‑size‑fits‑all. A young adult with mild hypertension might start on a low‑dose thiazide diuretic, while an older patient with heart failure may need an ACE inhibitor plus a beta blocker. The choice also hinges on side‑effect profiles: ACE inhibitors can cause a dry cough, beta blockers may bring fatigue, and calcium channel blockers sometimes lead to swelling in the ankles. Discussing these nuances with your doctor ensures you get a regimen that matches your lifestyle.
Beyond the pills, lifestyle factors influence how well these medicines work. Reducing sodium, staying active, and managing stress can boost drug effectiveness and sometimes let you lower the dose. Think of it as a partnership: the drug does the heavy lifting, but your daily habits keep the pressure down and protect your heart over the long run.
When you start a new blood pressure drug, monitoring is crucial. Most doctors advise checking your pressure at home at least twice a week, especially during the first month. Keep a log of any new symptoms—dizziness, unusual swelling, or persistent cough—and share it at follow‑up visits. This feedback loop lets the prescriber fine‑tune dosage or switch classes if needed.
In the sections below you’ll find detailed looks at each drug class, side‑effect management tips, and real‑world comparisons that help you decide which option fits your health goals. Whether you’re just diagnosed, switching meds, or helping a loved one understand their prescription, the articles ahead break down the science into easy‑to‑use guidance.
Hydrochlorothiazide vs Alternatives: A Practical Comparison
A clear, side‑by‑side look at Hydrochlorothiazide and its common alternatives, covering how they work, dosing, effectiveness, and key safety points for hypertension management.
Keep Reading