Amenorrhea Treatment: Options, Hormones, and Practical Tips
When facing amenorrhea treatment, the medical plan to bring back regular periods for women who miss them. Also called absence of menses therapy, it begins with finding out why periods stopped before picking the right fix.
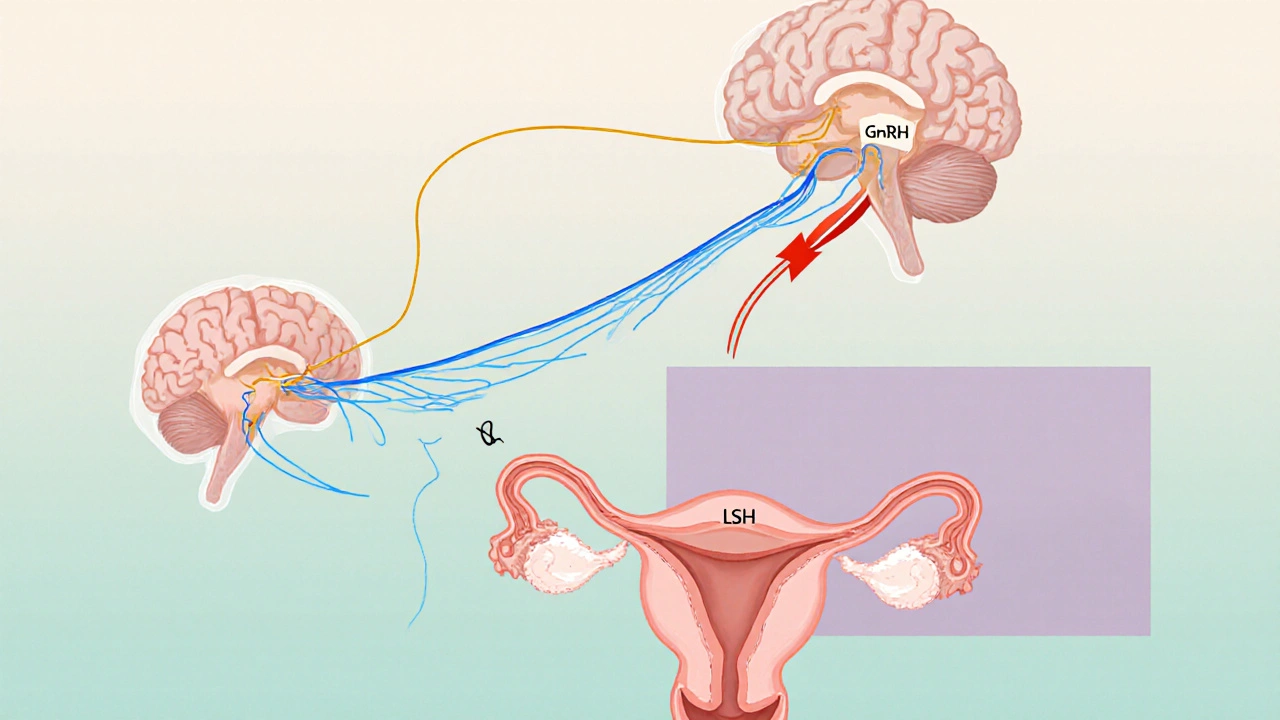
One of the biggest pillars of amenorrhea treatment is hormone therapy, using synthetic or natural hormones to replace what the body isn’t producing. Hormone therapy usually pairs two key hormones: estrogen, the hormone that builds the uterine lining and progestin, the synthetic version of progesterone that stabilizes the lining and triggers shedding. The combo works because amenorrhea often stems from low estrogen levels, and without that signal the body never prepares for a period.
How Underlying Causes Shape the Therapy
Think of amenorrhea treatment like fixing a car: you can’t just replace the battery without checking the alternator. Common causes—polycystic ovary syndrome (PCOS), thyroid disorders, excessive stress, or low body weight—each demand a slightly different approach. For PCOS, doctors may start with insulin‑sensitizing meds and then add hormone therapy. Thyroid‑related amenorrhea usually gets treated by normalizing thyroid hormone first, then addressing the menstrual gap. Lifestyle factors such as intense exercise or drastic dieting can be corrected with nutrition tweaks, which sometimes eliminates the need for drugs altogether.
Another widely used option is the oral contraceptive pill (OCP). It delivers a steady dose of estrogen and progestin, tricking the body into a monthly cycle even when natural production is off‑track. OCPs are especially handy when the root cause is unknown or when a woman needs reliable cycle control for birth planning. They also help with acne or hirsutism that often accompany hormonal imbalances.
When doctors need a more targeted estrogen boost, they might prescribe Premarin, a conjugated estrogen derived from pregnant mares, used to jump‑start the uterine lining or its synthetic cousin Estradiol, a bioidentical form of estrogen that mimics the body’s natural hormone. These are often paired with a short course of progestin like Provera, medroxyprogesterone acetate that ensures the lining sheds properly. The sequence—estrogen first, progestin later—mirrors the natural menstrual rhythm and reduces the risk of irregular bleeding.
For women who want to conceive, the drug Clomiphene, a selective estrogen receptor modulator that nudges the ovaries to release eggs can be part of the treatment plan. It’s often used after hormone therapy has re‑established a baseline cycle. The goal here isn’t just to bring back periods; it’s to create a fertile environment for pregnancy.
All these options share a common thread: they aim to restore the hormonal balance that drives the menstrual cycle. The choice depends on age, desire for pregnancy, severity of the hormone deficit, and any co‑existing health issues. A thorough lab workup—checking estradiol, progesterone, thyroid panels, and insulin levels—helps clinicians map the best route.
Below you’ll find a curated set of articles that dive deeper into each of these treatments. Whether you’re curious about the nuances of OCPs, need a side‑by‑side drug comparison, or want practical tips for lifestyle‑driven amenorrhea, the collection offers clear, actionable guidance to help you move forward with confidence.
Understanding Amenorrhea: Causes, Symptoms, and Treatments
A clear guide to amenorrhea that explains what it is, why periods stop, how to spot symptoms, get diagnosed, and choose effective treatments.
Keep Reading