Amenorrhea Cause Explorer
Potential Causes
Enter your information and click "Analyze Potential Causes" to see possible triggers for amenorrhea.
Hormonal Imbalances
Polycystic ovary syndrome (PCOS), thyroid disorders, hyperprolactinemia
Weight-Related Issues
Low body fat or rapid weight gain affecting estrogen production
Physical Stress
Intense exercise or chronic mental stress suppressing reproductive axis
Structural Problems
Uterine scarring or congenital anomalies blocking shedding
TL;DR
- Amenorrhea means no periods for three months or more.
- Common triggers include hormonal imbalances, stress, excessive exercise, low body weight, and medical conditions such as PCOS or thyroid disorders.
- Key symptoms are missed periods, infertility concerns, and possible signs of underlying disease.
- Diagnosis starts with a medical history, blood tests, and sometimes imaging.
- Treatment ranges from lifestyle changes to hormone therapy, depending on the root cause.
What Is Amenorrhea?
Amenorrhea is a medical condition characterized by the absence of menstrual periods for three consecutive months or longer in women of reproductive age. While it can be a temporary response to stress or weight loss, persistent amenorrhea often signals a deeper hormonal or health issue that needs attention.
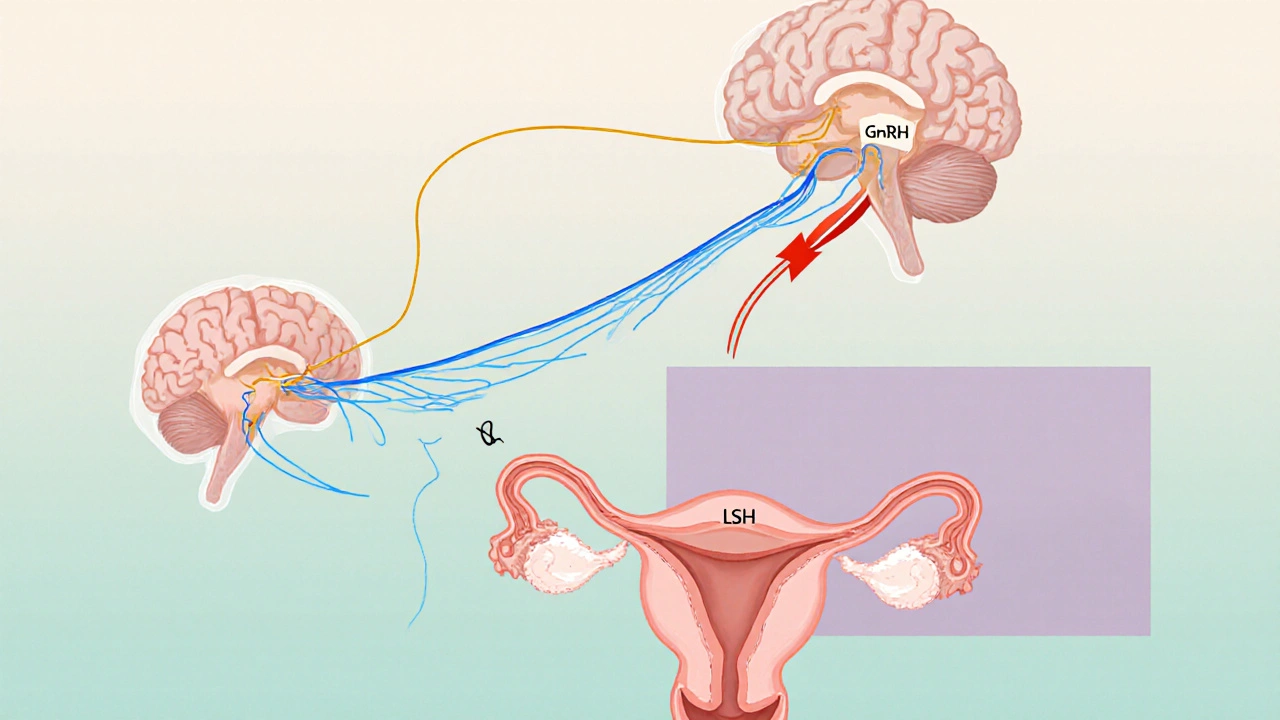
How the Hormonal System Controls Your Cycle
Understanding amenorrhea starts with the hypothalamic‑pituitary‑ovarian axis. The hypothalamus releases GnRH, prompting the pituitary gland to secrete FSH and LH. Those hormones stimulate the ovaries to produce estrogen and progesterone, which drive the monthly buildup and shedding of the uterine lining. Disruption at any point can halt periods.
Major Causes of Amenorrhea
There isn’t a one‑size‑fits‑all answer; most cases involve a mix of factors. Below are the most frequent culprits, grouped by category.
- Hormonal imbalances
- Polycystic ovary syndrome (PCOS) - excess androgen production can prevent ovulation.
- Thyroid disorders - both hyper‑ and hypothyroidism interfere with menstrual regulation.
- Hyperprolactinemia - elevated prolactin suppresses GnRH.
- Weight‑related issues
- Low body fat from restrictive diets or eating disorders (anorexia nervosa or bulimia) reduces estrogen production.
- Rapid weight gain can also trigger hormonal shifts, especially if it leads to insulin resistance.
- Excessive physical stress
- High‑intensity training or endurance sports increase cortisol, which suppresses the reproductive axis.
- Chronic mental stress has a similar effect.
- Structural or anatomical problems
- Uterine scarring (Asherman's syndrome) after surgery or infection can block shedding of the lining.
- Congenital uterine anomalies.
- Medications and medical treatments
- Some antipsychotics, chemotherapy, and hormonal contraceptives can temporarily stop periods.

Spotting the Symptoms
Besides the obvious missed periods, watch for these warning signs:
- Sudden weight loss or gain.
- Increasing hair growth on the face or chest (a sign of androgen excess).
- Acne or oily skin.
- Fatigue, mood swings, or depression.
- Painful pelvic area or abnormal vaginal discharge.
If any of these appear with a stopped cycle, it’s time to see a healthcare professional.
Diagnostic Workup: What Your Doctor Will Do
The goal is to pinpoint the root cause. Typical steps include:
- Medical history and physical exam - age, menstrual pattern, lifestyle, medication use.
- Blood tests
- FSH, LH, estradiol, prolactin, TSH, and free T4 to check pituitary and thyroid function.
- Androgen levels (testosterone, DHEA‑S) if PCOS is suspected.
- Pregnancy test - always rule out pregnancy first.
- Imaging
- Pelvic ultrasound to view ovarian morphology and uterine lining.
- MRI of the brain if a pituitary tumor is a concern.
- Additional assessments - bone density scan if amenorrhea has lasted over a year, as low estrogen can weaken bones.
Choosing the Right amenorrhea treatment
Treatment is personalized. Below is a quick guide to the most common approaches, followed by a side‑by‑side comparison.
| Treatment | How It Works | Typical Duration | Pros | Cons |
|---|---|---|---|---|
| Hormone Replacement Therapy (HRT) | Provides estrogen (and sometimes progesterone) to replace what the ovaries aren’t making. | 3-12 months, then reassess | Restores bone density, improves mood, may restart periods. | Risk of blood clots, requires monitoring. |
| Combined Oral Contraceptives (COC) | Delivers synthetic estrogen and progestin to regulate the cycle. | At least 6 months for stable cycle. | Highly effective, also manages acne and hirsutism. | May mask underlying cause, side effects like nausea. |
| Weight Management & Nutrition | Restores body fat levels to re‑establish normal estrogen production. | Varies; often 6-12 months. | Improves overall health, sustainable long‑term. | Requires discipline; progress can be slow. |
| Psychological Counseling / Stress Reduction | Reduces cortisol‑mediated suppression of the reproductive axis. | Ongoing; noticeable improvements in 3-6 months. | Addresses mental health, enhances quality of life. | May need concurrent medical therapy. |
| Surgical Correction (e.g., hysteroscopic adhesiolysis) | Removes uterine scar tissue that blocks shedding. | One‑time procedure; follow‑up for 6-12 months. | Can restore normal menstruation in Asherman's syndrome. | Invasive, risk of infection, not always successful. |
Choosing the right path often means combining options. For example, a woman with low body weight and PCOS may benefit from both nutritional counseling and a low‑dose COC.
Lifestyle Tweaks That Support Recovery
Even after medical treatment, everyday habits make a huge difference.
- Balanced diet - aim for 45‑55% carbs, 20‑25% protein, and healthy fats; include iron‑rich foods like leafy greens.
- Moderate exercise - 150 minutes of moderate aerobic activity per week is ideal; avoid excessive high‑intensity training.
- Stress management - mindfulness, yoga, or simple breathing exercises can lower cortisol.
- Adequate sleep - 7‑9 hours nightly supports hormone regulation.
- Regular check‑ups - track hormone levels every few months until cycles normalize.
When to Seek Immediate Medical Attention
If you notice any of the following, call your doctor right away:
- Severe pelvic pain or sudden heavy bleeding.
- Signs of thyroid trouble (rapid heartbeat, unexplained weight changes).
- Symptoms of anemia (fatigue, shortness of breath).
- Persistent mood swings or thoughts of self‑harm.

Frequently Asked Questions
Can stress alone cause amenorrhea?
Yes. Chronic stress raises cortisol, which can suppress the hypothalamic‑pituitary‑ovarian axis and stop periods. Reducing stress often helps restore cycles.
Is amenorrhea the same as menopause?
No. Menopause occurs naturally after age 45‑55 when the ovaries stop producing hormones. Amenorrhea can happen at any reproductive age and is usually due to an underlying condition.
How long does it take for periods to return after treatment?
It varies. Hormonal therapy can restart cycles within 1‑3 months, while lifestyle changes may take 6‑12 months. Regular monitoring is key.
Can I get pregnant while having amenorrhea?
It’s possible but unlikely, because ovulation usually stops when periods stop. However, sporadic ovulation can still occur, so using contraception if you’re not trying to conceive is wise.
Do birth control pills hide the real problem?
Birth‑control pills can regulate bleeding and mask symptoms, but they don’t cure the underlying cause. Doctors often use them while simultaneously treating the root issue.






18 Comments
Amenorrhea is a basic health issue that anyone can grasp without fancy jargon. Your body stops the monthly bleed when the hormonal signals get out of sync. Stress, extreme exercise, or low body fat can all pull the plug on those signals. Even a simple blood test can show whether thyroid or prolactin levels are off. If you’re not pregnant, missing three periods in a row is a red flag. Doctors will look at your diet, workout routine, and mental stress levels. Fixing the root cause usually brings the cycle back. In many cases, a balanced diet and a bit less cardio do the trick. If hormones are the problem, medication can reset the balance. The key is not to ignore the silence of your cycle.
Wow, another endless medical lecture 😒. People love to turn a simple missed period into a drama series. 🙄 If you’re stressed, just chill out – it’s not rocket science. And sure, let’s throw in an emoji for every hormone you’re missing. 🙃
From a physiological standpoint, the hypothalamic‑pituitary‑ovarian axis orchestrates the menstrual rhythm with remarkable precision. When stressors-be they psychological, nutritional, or kinetic-disrupt GnRH pulsatility, downstream FSH and LH secretion falters, leading to anovulation and hence amenorrhea. Thyroid dysfunction, hyperprolactinemia, and androgen excess further complicate the endocrine milieu. Clinicians typically employ a stratified diagnostic algorithm: comprehensive history, serum panels, and ultrasonography. Therapeutic interventions range from lifestyle modulation to targeted pharmacotherapy, each calibrated to the etiological nuance.
Totally feel you on the stress thing, it’s like your body just says nope to periods. I’ve seen friends drop their cycles after marathon training, and a few weeks of binge‑eating didn’t help either. The best hack is to dial back the over‑exertion and give yourself some real rest. It’s not just about losing weight, it’s about giving the hormones a breather.
In the grand tapestry of human physiology, the cessation of menstruation-amenorrhea-serves as a profound sentinel, heralding an underlying discord within the intricate endocrine symphony that governs reproductive vitality. One must first acknowledge that the hypothalamic‑pituitary‑ovarian axis functions as the maestro, conducting a cascade of gonadotropin‑releasing hormone (GnRH) pulses that orchestrate the secretion of follicle‑stimulating hormone (FSH) and luteinizing hormone (LH). When this delicate choreography is perturbed, whether by the inexorable grip of chronic psychosocial stress, the relentless march of excessive aerobic training, or the insidious whisper of caloric insufficiency, the downstream estrogenic milieu dwindles, and the endometrium remains unwrought. Moreover, the specter of polycystic ovary syndrome looms, its hyperandrogenic overtones casting a shadow that not only stymies ovulation but also fuels hirsutism and acne, thereby compounding the clinical picture. Thyroid dysregulation, whether hyperthyroidism’s accelerated metabolism or hypothyroidism’s sluggish cadence, further muddies the hormonal waters, demanding meticulous laboratory appraisal. In parallel, hyperprolactinemia, often an enigmatic byproduct of pituitary microadenomas or pharmacologic agents, exerts an inhibitory effect upon GnRH release, sealing the fate of the menstrual cycle. Structural anomalies, such as Asherman’s syndrome-a tragic sequela of intrauterine adhesions-can mechanically obstruct endometrial shedding, culminating in a sterile silence. The diagnostic odyssey, therefore, must be both comprehensive and methodical, encompassing a thorough anamnesis, judicious imaging-typically transvaginal ultrasonography-and a panel of serum assays that illuminate the hormonal tableau. Therapeutically, one must tailor interventions to the etiologic substrate: nutritional rehabilitation for low‑weight individuals, stress‑reduction modalities for the over‑strained psyche, and, when warranted, hormonal supplementation or contraceptive regimens to re‑establish cyclicity. Ultimately, the restoration of menses is not merely a cosmetic triumph but a herald of reclaimed homeostasis, safeguarding bone density, cardiovascular health, and psychosocial wellbeing.
Amenorrhea is a moral failing of neglecting one’s body health It is a reminder that personal responsibility must prevail The solution lies in disciplined lifestyle changes and rigorous medical supervision
Everyone says stress is the main cause but maybe it’s just an excuse for lazy doctors not digging deep enough
Hey! 🌟 Keep your chin up – many folks bounce back with the right nutrition and a gentle exercise plan. You’ve got this! 😊
yo i think its cool to remember that a quick blood test can show if ur thyroid or prolactin is off your body isnt that neat? also dont forget the importance of a good diet & rest – they really do help u get those cycles back.
Oh sure, because reading a three‑page medical article will instantly solve all your period woes – sarcasm aside, a balanced diet does beat a magic pill any day.
In short, if you’ve missed three menstrual cycles, rule out pregnancy first, then check thyroid, prolactin, and androgen levels. Lifestyle factors like extreme exercise or low body fat are common culprits. Treatment varies from diet adjustments to hormonal therapy depending on the cause.
Just stop stressing.
Ah, the classic “just relax” mantra – as if the universe cares about our calendar. Yet, a sprinkle of irony does remind us that sometimes the best medicine is a bit of perspective and a dash of sarcasm.
Let’s remember that each person’s journey with amenorrhea is unique, and compassion goes a long way. Supportive communities can offer both emotional encouragement and practical tips, making the path to recovery less lonely.
Check your iron levels and consider a vitamin D supplement – both can impact menstrual health.
Isn’t it amusing how the body decides to shut down a process that’s been so reliable for millennia? Yet, when you dig into the biochemistry, you see a cascade of feedback loops that can be tipped by something as simple as a missed meal or a marathon. The irony is that the very mechanisms designed to preserve reproductive potential become the Achilles’ heel when modern lifestyles push the limits. So, while we lament the lost periods, we should also marvel at the adaptability of our endocrine system – it’s both fragile and resilient in equal measure.
Sure, just add a dash of sarcasm to the treatment plan: “Take this hormone pill, and maybe your cycle will thank you 😉”. In all seriousness, a personalized approach works best.
Look amenorrhea is a result of many factor it is not only about stress it can be due to medical condition and diet so dont blame only one thing