Myasthenia Gravis is a chronic autoimmune disorder that weakens the skeletal muscles, especially those controlling eye movement, swallowing, and breathing. In people over 65, the disease often presents with subtle fatigue and higher risk of respiratory complications, making caregiver vigilance crucial.
Key Takeaways
- Monitor muscle strength daily and watch for signs of respiratory distress.
- Maintain a strict medication schedule; timing matters more than dosage size.
- Collaborate with a multidisciplinary team: neurologist, respiratory therapist, and physical therapist.
- Address caregiver stress proactively through support groups and respite care.
- Plan for emergency situations with a written crisis protocol.
Understanding the Disease Mechanism
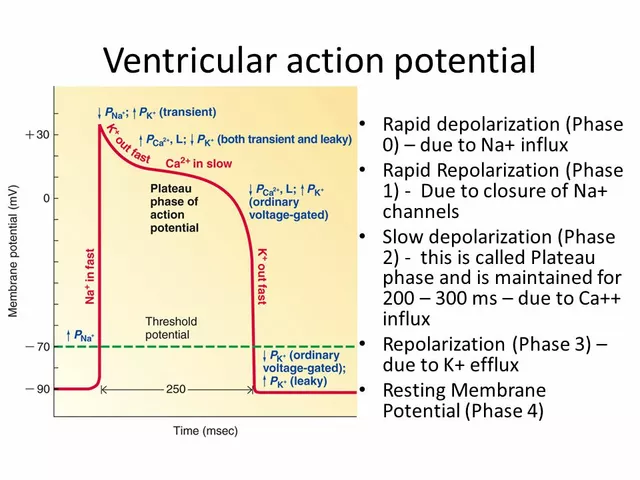
At its core, acetylcholine receptor antibodies target the neuromuscular junction, blocking the signal that tells muscles to contract. This blockage leads to the characteristic “fatigable weakness.” In the elderly, the thymus-a gland that helps train the immune system-often involutes, but residual thymic tissue can still fuel antibody production.
Common Symptoms in Older Adults
Older patients may not exhibit the classic ptosis (drooping eyelid) or double vision. Instead, look for:
- Generalized fatigue that worsens by day’s end.
- Difficulty chewing or swallowing, leading to weight loss.
- Shortness of breath during mild exertion.
- Occasional voice changes or hoarseness.
Because these signs overlap with age‑related conditions, a neurologist specializes in diagnosing and managing neuromuscular disorders should confirm the diagnosis with antibody testing and electromyography.
Medication Management
Two medication classes dominate treatment:
| Drug | Mechanism | Typical Onset | Dosing Frequency | Key Side Effects in Seniors |
|---|---|---|---|---|
| Pyridostigmine acetylcholinesterase inhibitor | Boosts acetylcholine levels at the neuromuscular junction | Minutes to hours | 3-4 times daily | Diarrhea, abdominal cramps, increased secretions |
| Azathioprine purine synthesis inhibitor (immunosuppressant) | Reduces antibody production over weeks | 6-12 weeks | Once daily | Liver toxicity, leukopenia, infection risk |
For seniors, the balance tips toward a lower pill burden, but Myasthenia Gravis care for seniors must still respect the faster relief provided by pyridostigmine while monitoring for gastrointestinal upset.
Safety Measures at Home
Because muscle weakness can affect swallowing and breathing, the home should be a low‑risk environment:
- Arrange eating utensils with larger handles to accommodate reduced grip strength.
- Keep a pulse oximeter portable device that measures blood oxygen saturation nearby; a reading below 92% warrants immediate medical attention.
- Install grab bars in the bathroom and consider a bedside chair with a back‑rest for nighttime breathing support.
- Educate all family members on the signs of a myasthenic crisis sudden respiratory failure requiring ventilatory support, such as rapid shallow breathing, difficulty speaking, or cyanosis.
Physical Therapy and Activity
Gentle, regular exercise can preserve muscle endurance without overtaxing fatigued fibers. A physical therapist creates tailored strength‑building programs for neuromuscular patients often recommends:
- Low‑impact aerobic activity (e.g., walking, stationary cycling) for 10‑15 minutes, twice daily.
- Isometric exercises focusing on neck, shoulder, and facial muscles, performed in short sets with ample rest.
- Balance drills to prevent falls, especially important when medication causes dizziness.
Track progress in a simple log: date, activity, duration, perceived exertion, and any worsening of symptoms.

Managing Caregiver Stress
Providing round‑the‑clock support can wear down even the most resilient caregiver. Strategies to stay balanced include:
- Scheduling regular respite-whether a trusted neighbor, adult‑day program, or paid caregiver-for a few hours each week.
- Joining an online support community focused on Myasthenia Gravis; peer stories often reveal practical hacks you won’t find in medical texts.
- Practicing brief mindfulness exercises (5‑minute breathing drills) during medication administration to stay calm and focused.
- Keeping a backup list of emergency contacts: neurologist, primary care physician, nearest hospital with an ICU capable of mechanical ventilation.
Creating a Crisis Action Plan
Even with optimal control, crises can happen. A written plan should contain:
- Exact times and doses of all medications, especially pyridostigmine and any steroids.
- Instructions for the caregiver to call emergency services if breathing becomes labored, with a brief script: ‘We have a patient with Myasthenia Gravis experiencing respiratory distress.’
- Location of the nearest hospital that treats neuromuscular emergencies.
- List of current comorbidities (e.g., hypertension, diabetes) that may influence acute treatment.
Review this plan with the whole care team quarterly; updates are often needed as the disease progresses or medication regimens change.
Advance Care Planning
Discussing future wishes isn’t about giving up; it’s about guaranteeing that the patient’s values guide medical decisions when they can’t speak for themselves. Topics include:
- Do‑Not‑Resuscitate (DNR) preferences.
- Intubation and mechanical ventilation preferences during a crisis.
- Legal documents: durable power of attorney, living will.
Engage a geriatrician or palliative‑care specialist to ensure that documentation meets local regulations.
Nutrition and Swallowing Support
Weakness in the oropharyngeal muscles can lead to aspiration pneumonia-a leading cause of hospitalization for seniors with MG. Steps to reduce risk:
- Schedule a bedside swallowing evaluation with a speech‑language pathologist.
- Prefer soft, easy‑to‑chew foods; avoid dry crackers or tough meats.
- Encourage upright sitting for at least 30 minutes after meals.
- Consider a thickened liquid supplement if thin fluids cause coughing.
Monitoring and Follow‑Up
Regular check‑ins keep the disease in check and catch subtle changes early. A typical schedule might be:
- Neurologist visit every 3‑6 months, with antibody titers checked annually.
- Pulmonary function tests once a year, or sooner if breathing worsens.
- Blood work for immunosuppressant levels every 4-6 weeks.
Document each visit in a shared binder or digital folder accessible to all caregivers.
Frequently Asked Questions
How often should I give pyridostigmine to an elderly patient?
The usual schedule is three to four times a day, spaced evenly (e.g., 8am, 12pm, 4pm, 8pm). Adjust timing around meals to reduce stomach upset, and always follow the prescribing doctor’s exact instructions.
What are early signs of a myasthenic crisis?
Watch for rapid shallow breathing, difficulty speaking full sentences, facial droop that worsens quickly, or a sudden drop in oxygen saturation below 92%. If any appear, call emergency services immediately.
Can immunosuppressants be safely used in people over 70?
Yes, but they require close monitoring. Regular blood tests for liver function and white‑blood‑cell counts are essential. Start at a low dose and titrate slowly, watching for infections.
What home equipment helps prevent falls for MG patients?
Grab bars in bathrooms, non‑slip mats, a sturdy bedside chair, and a walking aid (cane or walker) rated for the patient’s weight are all recommended.
How can I reduce caregiver burnout?
Schedule regular respite, join a support group, keep a daily log of tasks to identify patterns, and practice short mindfulness breaks. Remember, caring for yourself lets you care better for your loved one.


13 Comments
What a thorough walkthrough! The way you dissected the acetylcholine blockade, the nuanced medication timing, and the home safety checklist-it's practically a handbook, not just a Reddit post. I especially love the emphasis on pulse‑ox monitoring, because a subtle dip below 92 % can mean a lot, and early intervention is everything. Your suggestion to log activities with perceived exertion is gold; it transforms vague fatigue into actionable data, and that data can guide dose adjustments. Also, the crisis action plan script for EMS-brilliant, it removes hesitation when seconds count. Kudos for blending clinical precision with caregiver empathy, all in one tidy article.
Honestly, I think the whole “grab‑bars everywhere” thing is overkill for most seniors; a simple chair lift does the trick.
Absolutely loving the depth here! 😄 The tip about larger utensil handles is something I tried with my aunt and she swears by it now. Keeping a bedside oxygen monitor? Game‑changer. Also, the suggestion to involve a speech‑language pathologist early can cut down aspiration risks dramatically. Thanks for the solid, practical guide-feels like a lifeline for anyone juggling meds and mobility.
Too much detail, not enough focus on actual caregiver burnout.
While conciseness is valuable, omitting the stress‑management strategies could leave caregivers feeling isolated. A balanced approach would integrate both.
Reading through the protocol reminded me of the importance of redundancy in care plans. Having both a written script and a digital copy on a phone ensures you’re never caught off guard. Also, rotating caregivers weekly can reduce fatigue, which aligns with the article’s emphasis on respite. The suggestion to log each visit in a shared binder is practical; digital folders work too, especially when family members live far away. Lastly, integrating a low‑impact aerobic routine twice daily seems doable without overtaxing the patient.
We should also push for local community health workers to be trained on Myasthenia Gravis; importing expertise is costly and unnecessary when our own nurses can be upskilled. A home‑grown support network strengthens resilience. Don’t rely solely on distant specialists.
Looks like a lot of fluff.
While it may seem lengthy, each section provides a safety net for seniors; ignoring them could be risky.
From a clinical perspective, the article adeptly delineates the pathophysiology of Myasthenia Gravis, emphasizing the role of acetylcholine receptor antibodies in disrupting neuromuscular transmission. The pharmacologic dichotomy between pyridostigmine, a rapid acetylcholinesterase inhibitor, and azathioprine, a slow‑acting immunosuppressant, is clearly articulated, which is crucial for dose‑timing optimization in geriatric cohorts. Moreover, the recommendation to employ pulse‑oximetry as a bedside surveillance tool aligns with evidence‑based thresholds for impending respiratory compromise (SpO₂ < 92 %). The integration of multidisciplinary care-neurology, pulmonology, physiotherapy, and speech‑language pathology-mirrors best‑practice models, fostering comprehensive symptom management. Home safety modifications, such as grab bars and non‑slip flooring, are not merely ergonomic; they constitute primary prevention against fall‑related morbidity. The article’s emphasis on caregiver respite acknowledges the psychosocial dimension of chronic disease, a factor often underrepresented in clinical guidelines. Additionally, the proposed crisis action plan script for emergency medical services enhances communication efficiency during high‑stress scenarios. The suggestion to maintain a detailed activity log serves both as a self‑monitoring instrument for patients and a data repository for clinicians adjusting therapeutic regimens. Nutritional considerations, particularly the avoidance of dry foods and the utilization of thickened liquids, mitigate aspiration risk-a leading cause of hospital admission in this demographic. The schedule of quarterly neurologist visits with annual antibody titration ensures longitudinal disease surveillance while balancing healthcare resource utilization. Pulmonary function testing at six‑month intervals provides an objective metric for lung capacity decline, informing ventilatory support decisions. The article rightly cautions about immunosuppressant‑induced leukopenia, advising regular complete blood counts to preempt opportunistic infections. From an ethical standpoint, the discussion on advance directives and DNR preferences underscores patient autonomy in end‑of‑life care planning. The inclusion of mindfulness techniques for caregivers introduces a low‑cost, high‑yield strategy to alleviate burnout. Finally, the comprehensive nature of this guide makes it a valuable adjunct to standard patient education handouts, bridging the gap between specialist recommendations and real‑world caregiving implementation.
The risk stratification algorithm presented, while robust, fails to address comorbidity interaction effects, particularly with polypharmacy in octogenarians. A Bayesian inference model could refine predictive accuracy for crisis onset. Nevertheless, the current framework offers a solid baseline for iterative improvement.
Interesting points on medication timing; I wonder if extended‑release pyridostigmine formulations could reduce dosing frequency for seniors.
Yeah, extended‑release could def help, but gotta watch for side‑effects-patients might still need to split doses if they feel weak later in the day.