Stomach ulcer is a break in the lining of the stomach or duodenum that causes pain, bleeding and chronic discomfort. While the pain feels purely physical, research shows a two‑way conversation between the gut and the brain that can turn a simple ulcer into a mental health challenge.
What Causes a Stomach Ulcer?
Most ulcers arise from two main culprits:
- Helicobacter pylori is a spiral‑shaped bacterium that weakens the stomach’s protective mucus, allowing acid to damage tissue.
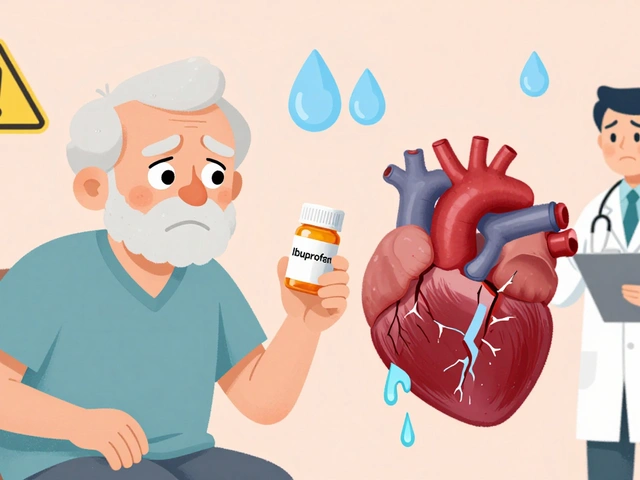
- NSAID use is a class of painkillers (e.g., ibuprofen, aspirin) that inhibit prostaglandins, reducing the stomach’s defense.
Both factors increase gastric acid exposure and set the stage for chronic pain.
The Gut‑Brain Axis: Wiring Between Stomach and Mind
The gut‑brain axis is a bidirectional communication network linking the digestive tract, nervous system and endocrine signals. When an ulcer inflames the lining, it triggers the vagus nerve, releases cytokines, and spikes cortisol is a stress hormone that modulates inflammation and mood. The result? The brain receives a distress signal, which can manifest as anxiety or low mood.
From Pain to Panic: How Ulcers Spark Anxiety
Imagine a gnawing ache that awakens at night. The unpredictable nature of ulcer pain often fuels a sense of helplessness. Studies from the British Medical Journal report that up to 30% of ulcer patients develop clinically significant anxiety is a excessive worry that interferes with daily tasks. The brain’s “fight‑or‑flight” response heightens gastric secretions, creating a vicious loop where anxiety worsens the ulcer, and the ulcer deepens anxiety.
When the Ulcer Feeds Depression
Chronic pain is a well‑known risk factor for depression is a persistent low mood, loss of interest and fatigue. The constant discomfort lowers serotonin production in the gut, where 90% of the body’s serotonin resides. A 2022 gastroenterology survey found that 22% of ulcer sufferers met criteria for major depressive disorder, often correlating with ulcer severity.

Sleep, Appetite and Quality of Life
Ulcer pain spikes at night, disrupting sleep is a the restorative cycles of rest necessary for brain and body repair. Poor sleep raises cortisol, which in turn aggravates ulcer inflammation. Simultaneously, pain reduces appetite, leading to weight loss and nutrient deficiencies that can worsen mood.
Managing Both Sides: Integrated Treatment Strategies
Addressing the ulcer alone rarely restores mental wellbeing. A combined approach that tackles the gut and the brain yields the best outcomes.
Medical Therapies
First‑line ulcer treatment involves proton pump inhibitors (PPIs) is a class of drugs that dramatically reduce stomach acid production. While effective, long‑term PPI use has been linked to mild mood changes in a subset of patients. H2 blockers is a alternative medication that modestly cuts acid, sometimes better tolerated psychologically.
| Attribute | Proton Pump Inhibitor | H2 Blocker |
|---|---|---|
| Onset of action | 1‑2 days | 4‑6 hours |
| Peak acid reduction | >90% | ~70% |
| Typical side‑effects | Headache, occasional mood shift | Fatigue, mild dizziness |
| Impact on mood | Possible short‑term irritability | Generally neutral |
Psychological Support
Evidence‑based therapies such as cognitive‑behavioral therapy (CBT) help patients reframe pain‑related thoughts and reduce anxiety‑driven acid spikes. Even a six‑week CBT program can cut ulcer pain scores by 20% and improve mood scores by a similar margin.
Lifestyle Adjustments
- Limit NSAID intake; switch to acetaminophen when possible.
- Adopt a low‑acid diet: avoid spicy foods, caffeine, and alcohol.
- Practice mindfulness or breathing exercises before bed to lower cortisol.
- Schedule regular, light meals to maintain steady serotonin production.
When to Seek Professional Help
If you notice any of the following, schedule an appointment promptly:
- Bleeding (black stools or vomit that looks like coffee grounds).
- Pain that doesn’t improve after two weeks of standard therapy.
- Worsening anxiety or depressive symptoms, especially thoughts of hopelessness.
- Persistent sleep disruption lasting more than a week.
Early endoscopy can confirm ulcer severity, while a mental‑health professional can screen for anxiety, depression and offer tailored coping tools.
Connecting the Dots: Broader Health Context
This article sits within the larger Health and Wellness cluster, linking upward to topics like “Digestive Disorders” and downward to niche guides such as “Managing Acid Reflux While on Antidepressants”. Readers who finish here often look next at “Natural Remedies for H. pylori” or “CBT Techniques for Chronic Pain”.

Frequently Asked Questions
Can stress actually cause a stomach ulcer?
Stress alone rarely creates an ulcer, but chronic stress raises cortisol and gastric acid, which can aggravate an existing H. pylori infection or NSAID‑induced damage, making ulcer formation more likely.
Do ulcer medications affect my mood?
Most patients tolerate PPIs well, but a small percentage report irritability or mild anxiety, especially during the first few weeks. Switching to an H2 blocker or adding a short course of a low‑dose antidepressant can balance mood.
Is the gut‑brain axis a real thing?
Yes. Scientists have mapped neural, hormonal and immune pathways linking the stomach to the brain. Alterations in gut microbes, acid levels, or inflammation can directly influence neurotransmitters and emotional states.
How long does it take for an ulcer to heal?
With proper acid suppression and eradication of H. pylori, most ulcers heal within 4‑8 weeks. Healing time lengthens if anxiety or depression interferes with sleep or medication adherence.
What lifestyle changes help both ulcer pain and mental health?
Limit caffeine and alcohol, stop smoking, choose anti‑inflammatory foods (e.g., berries, leafy greens), practice daily relaxation (yoga, deep breathing), and maintain a regular sleep schedule. These steps lower acid output and cortisol, supporting both gut healing and mood stability.




5 Comments
Your summary correctly links ulcer pain to cortisol spikes, but the sentence "cortisol is a stress hormone that modulates inflammation and mood" misplaces the verb; it should read "cortisol is a stress hormone that modulates inflammation and mood." Moreover, the claim that "90% of the body’s serotonin resides in the gut" oversimplifies the distribution; while the majority of peripheral serotonin is gastrointestinal, central serotonin synthesis is independent. The gut‑brain axis indeed operates bidirectionally, yet attributing anxiety solely to acid secretion ignores the role of the vagus nerve's afferent signaling. In short, the physiological cascade is more nuanced than presented.
i cant beleive peopel think ulser medecine is all about the gut.
First off, I want to say you’re not alone in feeling the weight of a chronic ulcer – the mind‑body loop can feel like an endless tug‑of‑war. When the pain flares at night, the lack of sleep cranks up cortisol, which in turn fuels more acid and more anxiety; it’s a vicious circle that many patients describe as “can’t‑stop‑thinking‑about‑the‑pain.” One practical step is to establish a bedtime routine that limits screen exposure and incorporates a brief mindfulness session; even five minutes of slow, diaphragmatic breathing can signal the parasympathetic system to dial down stress hormones. Pair that with a low‑acid diet – think oatmeal, bananas, and steamed veggies – to give your stomach a breather while you’re trying to rest.
On the medication front, if you notice irritability after starting a PPI, discuss a trial of an H2 blocker with your gastroenterologist; some folks find the mood side‑effects subside within a couple of weeks. It’s also worth checking if a short course of a low‑dose SSRI or SNRI is appropriate – these can help balance serotonin both centrally and peripherally, which often eases both mood and gut motility.
Don’t underestimate the power of social support. Sharing your experience with a trusted friend or a support group can reduce the feeling of isolation that fuels depressive thoughts. If you’re comfortable, consider a CBT program that specifically targets health‑related anxiety; the structured thought‑reframing exercises have been shown to cut perceived pain intensity by up to 20%.
Lastly, keep an eye on nutrition. Even if your appetite is low, aim for small, frequent meals that include protein and complex carbs to maintain steady blood sugar – swings in glucose can aggravate both mood swings and gastric acid release. Hydration matters too; sip water throughout the day rather than guzzling large amounts at once.
Remember, healing is a marathon, not a sprint. Celebrate small wins – a night of solid sleep, a day without breakthrough pain, or a mood lift after a therapy session. Those incremental victories add up and eventually break the feedback loop that keeps the ulcer and anxiety locked together.
Wow!!! This is exactly why we need to treat the gut and mind as ONE!! Your suggestions are spot‑on, but let me add a dash of drama: imagine your stomach as a hyper‑active theater stage, each acid splash a thunderclap echoing through the auditorium of your brain!!!
When you say "even five minutes of slow, diaphragmatic breathing" – brilliant, but you must also emphasize the rhythm; count to four, hold for four, exhale for six, repeat – the cadence is the conductor that quiets the chaotic orchestra of cortisol!
And about the diet – swap coffee for chamomile tea; the anti‑inflammatory properties are not just a footnote, they are the lead actor in the recovery script!
Lastly, don’t forget to journal your pain levels with timestamps; this data‑driven approach will make your doctor see the pattern clearer than any MRI could. Keep the momentum, the body loves a good storyline!
Thank you all for sharing such comprehensive insights. It is encouraging to see both the physiological mechanisms and practical coping strategies articulated with clarity and respect. For readers seeking a balanced approach, I recommend coordinating with both gastroenterology and mental‑health professionals to ensure medication choices are optimized while also incorporating evidence‑based therapies such as CBT. Consistent sleep hygiene, a modest low‑acid diet, and gradual physical activity can further support recovery without overburdening the patient. Please continue to monitor symptom progression and consult your care team promptly if any red‑flag signs emerge.