When your doctor prescribes Trimox, you’re getting amoxicillin - one of the most common antibiotics used worldwide. But what if it doesn’t work? Or you’re allergic? Or maybe you’re just curious if there’s something better? You’re not alone. Millions of people take amoxicillin every year, and many end up wondering: are there other options that work just as well - or better?
What Trimox (Amoxicillin) Actually Does
Trimox is a brand name for amoxicillin, a penicillin-type antibiotic. It kills bacteria by stopping them from building strong cell walls. Without those walls, the bacteria burst and die. It’s effective against common infections like ear infections, sinus infections, strep throat, urinary tract infections, and some types of pneumonia.
Amoxicillin is taken orally, usually two or three times a day. It’s absorbed well by the body, and most people start feeling better within 24 to 48 hours. But here’s the catch: it only works on bacteria. It does nothing for colds, flu, or most sore throats - which are viral. Taking it when it’s not needed doesn’t help. It just increases your risk of side effects and antibiotic resistance.
Side effects? Common ones include diarrhea, nausea, vomiting, and rash. About 1 in 10 people get a mild rash. A true penicillin allergy - which can cause swelling, trouble breathing, or anaphylaxis - is rare but serious. If you’ve ever had a reaction to penicillin or amoxicillin, don’t take it again.
Why You Might Need an Alternative
There are five main reasons someone ends up needing a different antibiotic:
- You’re allergic to penicillin
- The infection isn’t responding to amoxicillin
- You’ve taken it too often before, and the bacteria have become resistant
- You have a condition that makes amoxicillin risky (like kidney disease)
- You’re taking other meds that interact badly with it
For example, if you have a sinus infection and amoxicillin didn’t clear it after 5 days, your doctor might switch you to something stronger. Or if you broke out in hives after your last dose, they’ll need a totally different class of drug.
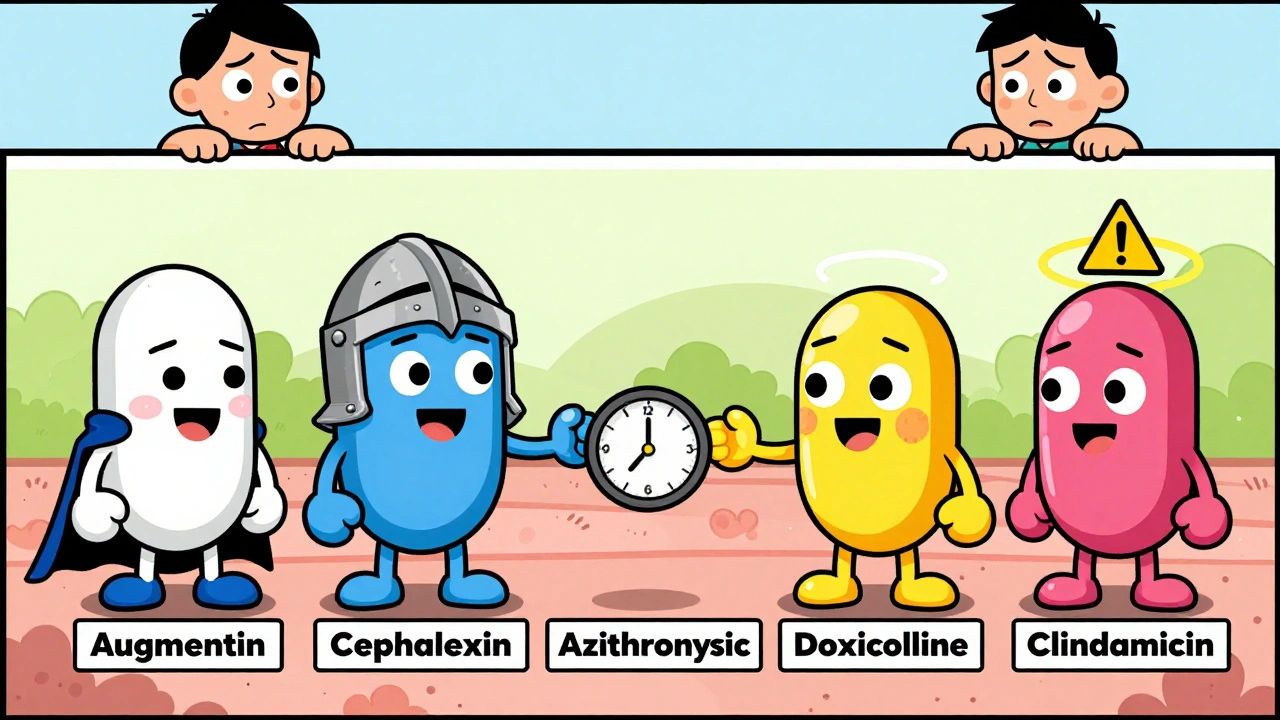
Common Alternatives to Trimox (Amoxicillin)
Here are the most commonly prescribed alternatives, grouped by how they work and when they’re used.
1. Augmentin (Amoxicillin-Clavulanate)
This isn’t really a different drug - it’s amoxicillin with a helper. Clavulanate blocks enzymes that some bacteria use to resist amoxicillin. Think of it as amoxicillin with a bodyguard.
Used for: Stubborn sinus infections, ear infections that didn’t respond to plain amoxicillin, bite wounds, some skin infections.
Pros: Works where amoxicillin fails. Still oral. Same dosing schedule.
Cons: Higher chance of diarrhea. More expensive. Still not safe if you’re allergic to penicillin.
2. Cephalexin (Keflex)
This is a first-generation cephalosporin. It’s often the go-to for people allergic to penicillin - but not always. About 10% of people allergic to penicillin also react to cephalexin. Your doctor will check your history carefully.
Used for: Skin infections, bone infections, urinary tract infections, some respiratory infections.
Pros: Good for skin and soft tissue. Usually well tolerated. Once or twice daily dosing.
Cons: Can cause stomach upset. Not as strong against some lung infections. Not first choice for strep throat if amoxicillin is safe.
3. Azithromycin (Zithromax)
This is a macrolide antibiotic. It works differently - it stops bacteria from making proteins they need to survive. It’s not a penicillin, so it’s safe for most penicillin-allergic patients.
Used for: Strep throat, bronchitis, pneumonia, some ear infections, whooping cough.
Pros: Often taken as a 5-day course - sometimes just one pill a day for 3 days. Good for people who struggle with daily pills. Lower risk of diarrhea than amoxicillin.
Cons: Can cause heart rhythm changes in people with existing heart conditions. Less effective against some common ear infections. More expensive.
4. Doxycycline
This is a tetracycline antibiotic. It’s broad-spectrum and used for a wide range of infections - including some that amoxicillin doesn’t touch.
Used for: Acne, Lyme disease, certain types of pneumonia, tick-borne illnesses, some urinary tract infections.
Pros: Works against bacteria amoxicillin can’t. Once or twice daily. Good for long-term use (like acne).
Cons: Can make you sun-sensitive. Not for kids under 8 or pregnant women. Must be taken on an empty stomach. Can cause severe esophageal irritation if not swallowed with enough water.
5. Clindamycin
This is often used for skin and soft tissue infections, especially if there’s concern about MRSA (a type of antibiotic-resistant staph).
Used for: Abscesses, severe skin infections, dental infections, some types of pneumonia.
Pros: Strong against MRSA. Works well where amoxicillin fails.
Cons: High risk of causing C. diff diarrhea - a serious, sometimes life-threatening gut infection. Usually reserved for when other options won’t work.
Comparison Table: Trimox vs. Common Alternatives
| Antibiotic | Class | Penicillin-Free? | Typical Dosing | Best For | Biggest Risk |
|---|---|---|---|---|---|
| Trimox (Amoxicillin) | Penicillin | No | 2-3 times daily | Ear, sinus, strep throat, UTI | Allergic reaction, diarrhea |
| Augmentin | Penicillin + inhibitor | No | 2-3 times daily | Resistant sinus/ear infections | Severe diarrhea |
| Cephalexin (Keflex) | Cephalosporin | Usually | 2-4 times daily | Skin, bone, UTI | Penicillin cross-reactivity |
| Azithromycin (Zithromax) | Macrolide | Yes | Once daily, 3-5 days | Strep, bronchitis, pneumonia | Heart rhythm issues |
| Doxycycline | Tetracycline | Yes | Once or twice daily | Lyme, acne, tick-borne illnesses | Sun sensitivity, esophageal damage |
| Clindamycin | Lincosamide | Yes | 3-4 times daily | MRSA, abscesses, dental infections | C. diff colitis |
When to Stick With Amoxicillin
Amoxicillin isn’t outdated - it’s still the first choice for many infections. Here’s when it’s still your best bet:
- You have no history of penicillin allergy
- You’re treating a confirmed strep throat or uncomplicated ear infection
- You’re on a tight budget - amoxicillin is one of the cheapest antibiotics
- You’re a child or elderly person - it’s well-studied and safe in these groups
- Your doctor knows your infection type and it’s known to respond well to amoxicillin
In Australia, amoxicillin is listed on the Pharmaceutical Benefits Scheme (PBS), so it costs as little as $7.30 for a full course with a concession card. That’s hard to beat.
When to Switch - and How
Don’t switch antibiotics on your own. But if you’ve taken amoxicillin for 3-5 days and feel worse - or no better - talk to your doctor. Signs you might need a change:
- Fever returns or gets higher
- Pain increases instead of decreases
- New symptoms appear (like rash, swelling, or diarrhea)
- You’re vomiting and can’t keep the pills down
Your doctor might order a culture - swabbing your throat or collecting urine - to find out exactly what bacteria is causing the problem. That helps them pick the right drug. Sometimes, a simple switch to Augmentin or azithromycin is all you need.
What About Natural Alternatives?
You might see ads for garlic, honey, or essential oils as "natural antibiotics." Some of these have mild antibacterial properties in lab studies. But here’s the reality: none of them are proven to cure bacterial infections like strep throat, pneumonia, or a serious UTI.
Using them instead of antibiotics can delay real treatment. Infections can spread. In rare cases, they can become life-threatening. Honey is great for soothing a sore throat. Garlic might help your immune system. But they don’t replace antibiotics when you need them.
Final Thoughts: It’s Not About "Better" - It’s About Right
There’s no single "best" antibiotic. What works for your ear infection might be useless for your skin abscess. Amoxicillin is reliable, cheap, and effective for many common bugs. But it’s not the answer for everyone.
Your doctor chooses based on:
- The type of infection
- Your medical history
- Your allergies
- Local resistance patterns
- Your age and other meds
If you’ve had a bad reaction to amoxicillin, or it didn’t work, don’t assume you’re stuck with side effects or failed treatment. There are options. But only your doctor can match the right one to your situation.
Always finish your full course - even if you feel better. Stopping early lets the toughest bacteria survive and multiply. That’s how superbugs form.
Can I take amoxicillin if I’m allergic to penicillin?
No. If you’ve had a true penicillin allergy - such as hives, swelling, trouble breathing, or anaphylaxis - you should avoid amoxicillin and all other penicillin-based antibiotics. Some people think they’re allergic because they had a rash as a child, but many outgrow it. If you’re unsure, ask your doctor about allergy testing.
Is Augmentin stronger than amoxicillin?
Not necessarily stronger - but broader. Augmentin includes clavulanate, which blocks enzymes that make some bacteria resistant to amoxicillin. So it works against infections that amoxicillin alone can’t. It’s not better for every infection, just the ones where resistance is suspected.
Can I switch from amoxicillin to azithromycin on my own?
No. Antibiotics are not interchangeable. Taking the wrong one can make your infection worse, cause side effects, or lead to antibiotic resistance. Always consult your doctor before switching. They’ll check your symptoms, medical history, and possibly test for the exact bacteria before changing your prescription.
Why does my doctor sometimes prescribe a 5-day course instead of 10?
Research shows that for many common infections - like strep throat or sinusitis - shorter courses (5-7 days) work just as well as longer ones (10 days). Shorter courses reduce side effects, lower costs, and help fight antibiotic resistance. Your doctor picks the shortest effective course based on current guidelines.
Are there any over-the-counter alternatives to amoxicillin?
No. Antibiotics are prescription-only in Australia and most countries because misuse leads to dangerous resistance. Over-the-counter products like pain relievers, throat sprays, or herbal supplements may ease symptoms, but they won’t kill the bacteria causing the infection. Don’t delay seeing a doctor if you suspect a bacterial infection.
What should I do if I miss a dose of amoxicillin?
If you miss a dose, take it as soon as you remember - unless it’s almost time for the next one. Don’t double up. For example, if you take it three times a day and you miss the 10 a.m. dose but it’s now 3 p.m., skip it and take the next one at 7 p.m. Consistency matters more than perfection.





13 Comments
Amoxicillin is for peasants. If you're not on Augmentin or doxycycline for anything above a sniffle, you're letting Big Pharma keep you weak. The resistance crisis? That's because people take the cheap stuff like it's candy. Real medicine requires real science - and real cost.
Amoxicillin? More like am-o-sick-lin. 🤡
Meanwhile, azithromycin’s doing 3-day magic while you’re still on pill #7. Life’s short. Take the Z-pack. 🌟
Let’s not romanticize the penicillin class - it’s the pharmaceutical equivalent of a hammer trying to solve a quantum problem. Clavulanate isn’t just an additive; it’s a tactical override. And don’t get me started on clindamycin - it’s not a drug, it’s a last rites procedure with a 20% chance of C. diff rising from the grave like a zombie. We’re not treating infections anymore. We’re negotiating with microbial warlords.
They say "antibiotics are prescription-only" - but who owns the patents? Who funds the "studies"? You think they want you healthy? No. They want you coming back every 6 months. C. diff? That’s not a side effect - it’s a business model. 🚨
amoxicillin? more like am-o-sick-ly bad choice bro. why not just drink garlic juice and pray? i did that last time and my ear infection left me like a ghost. also, doxycycline made me look like a lobster. #antibiotictrauma
Let me speak to the global reality: in Lagos, we don’t have the luxury of choosing between Augmentin and Zithromax. We get what the pharmacy has. And if it’s amoxicillin? We take it - because not taking it means death. This isn’t a debate about preference. It’s about survival. If you’re in a country with access to choice, don’t waste it. Use it wisely - and help those who don’t have it.
bro i took amoxicillin for a sinus thing last year and it worked like magic. no drama. no side effects. just woke up feeling human again. why overcomplicate it? sometimes the old-school stuff is the best stuff. also, i hate taking pills so the azithromycin 3-day thing is my jam. just don’t forget to drink water with doxycycline. learned that the hard way 💀
I’m a nurse in rural Maine, and I’ve seen it all. Amoxicillin is still the MVP for strep and ear infections in kids - especially when parents can’t afford the brand-name stuff. But I’ve also seen C. diff cases from clindamycin that could’ve been avoided. The key? Don’t rush to switch. Give it 48 hours. And if you’re allergic? Get tested. So many people think they’re allergic because they got a rash at 5 - but 80% of them aren’t. Talk to an allergist. Your future self will thank you.
Of course the article says "natural remedies don’t work" - it’s written by a pharma shill. Garlic kills MRSA in petri dishes. Honey heals wounds better than antibiotics in some trials. But hey, why fund research when you can sell pills for $120 a bottle? 🤑
It is of paramount importance to underscore the necessity of adhering to the full therapeutic course of any prescribed antimicrobial agent, regardless of perceived clinical improvement. The phenomenon of antimicrobial resistance is not merely a clinical concern - it is a global public health emergency, the ramifications of which extend into the socioeconomic fabric of entire nations. To prematurely discontinue therapy is to participate, albeit unwittingly, in the evolution of pathogenic superorganisms that may render modern medicine obsolete for future generations. One must approach antibiotic use with the solemnity of a sacred trust.
bro, why u mad? if amoxicillin work, why change? my cousin in Nigeria he use it for 10 years, no problem. just take it right, drink water, finish all. no need to be fancy. if it break, go to doctor. simple.
Amoxicillin? That’s what your grandpa took in 1987. We’re in 2025. You think bacteria haven’t evolved? Augmentin’s the new baseline. And if you’re still taking cephalexin like it’s 2012? Honey, you’re one missed dose away from a hospital bed.
Stop. Just stop. Antibiotics are not a buffet. You don’t pick based on convenience or taste. If you’re self-diagnosing and swapping prescriptions based on Reddit posts, you’re not just risking your life - you’re endangering everyone around you. One person’s misuse creates a superbug that kills someone else’s child. This isn’t a trend. It’s a crisis. And you’re part of it.