Celebrex vs NSAID Alternatives Comparison Tool
Select an NSAID from above to view detailed comparison information.
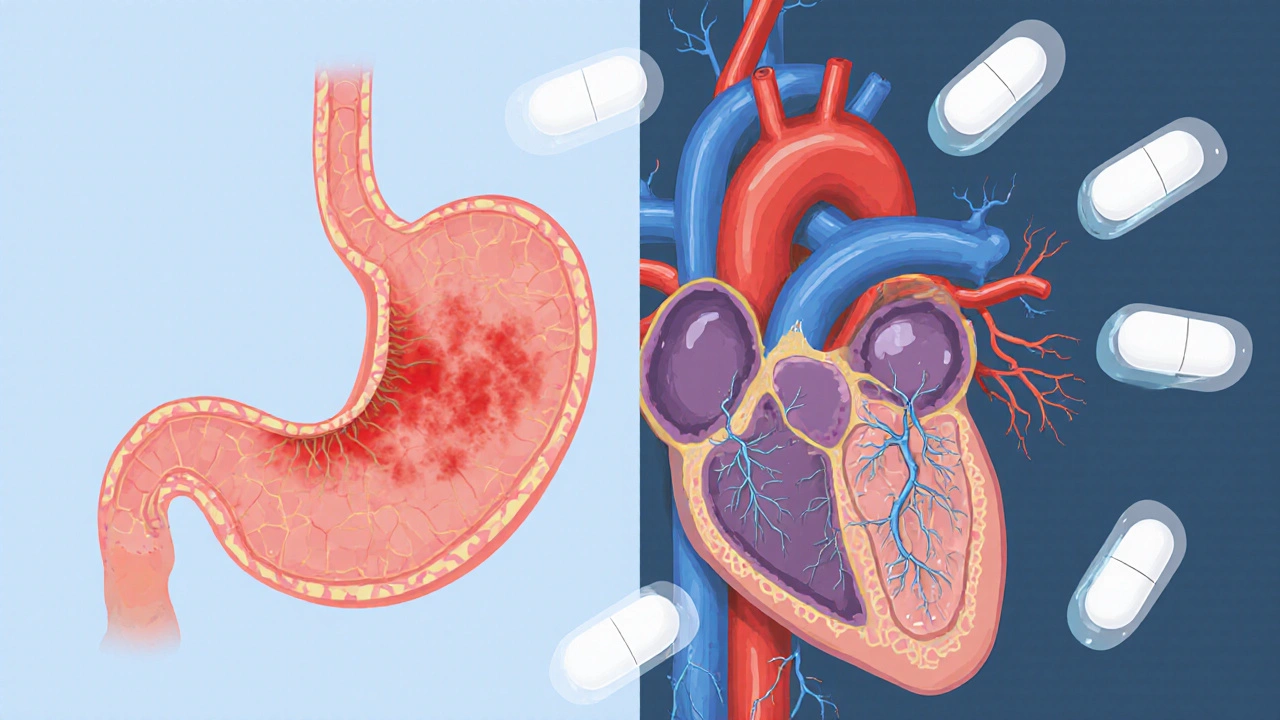
GI Risk
Lower risk with Celebrex and Meloxicam
Higher risk with Ibuprofen, Naproxen, and Diclofenac
CV Risk
Higher risk with Celebrex and Diclofenac
Lower risk with Naproxen and Aspirin
Cost
Most affordable: Ibuprofen, Naproxen
Most expensive: Celebrex (brand)
When it comes to managing chronic joint pain, many people wonder if Celebrex is the right choice or if other over‑the‑counter options might work better. This guide breaks down what makes Celebrex unique, how it stacks up against the most common alternatives, and what factors should guide your decision.
Key Takeaways
- Celebrex is a COX‑2‑selective NSAID designed to reduce inflammation with lower stomach irritation than traditional NSAIDs.
- Ibuprofen, naproxen, diclofenac, meloxicam, and aspirin are the main non‑selective NSAIDs often considered as alternatives.
- Cardiovascular risk is higher with Celebrex and some other COX‑2 inhibitors, while gastrointestinal (GI) risk is higher with non‑selective NSAIDs.
- Cost varies widely; Celebrex is usually pricier than generic ibuprofen or naproxen.
- Choosing the right drug depends on your specific condition, existing health issues, and how you tolerate side effects.
What is Celebrex?
Celebrex belongs to a class called COX‑2 inhibitors drugs that specifically block the cyclooxygenase‑2 enzyme, which drives inflammation and pain. By targeting COX‑2 and sparing COX‑1, the drug aims to protect the stomach lining while still providing strong anti‑inflammatory effects.
The active ingredient, celecoxib is a synthetic compound approved by the FDA in 1998 for arthritis and acute pain. Typical doses range from 100mg once daily for osteoarthritis to 200mg twice daily for acute gout attacks.
How Celebrex Works
COX‑2 is an enzyme that ramps up production of prostaglandins-chemicals that cause swelling, fever, and pain. Celebrex binds to the COX‑2 active site, preventing prostaglandin synthesis at sites of inflammation. Because COX‑1, which protects the stomach lining and supports platelet function, remains mostly untouched, the drug theoretically causes fewer stomach ulcers.
However, COX‑2 also plays a role in maintaining the balance of blood clotting factors. Inhibiting it can shift that balance, which explains the observed increase in cardiovascular events for some patients.
Common Alternatives to Celebrex
Below are the most frequently used NSAIDs that patients consider instead of Celebrex. Each has its own profile of effectiveness, side‑effect risk, and cost.
- Ibuprofen a widely available NSAID that blocks both COX‑1 and COX‑2 enzymes (e.g., Advil, Motrin).
- Naproxen another non‑selective NSAID known for its longer half‑life, sold as Aleve and generic versions.
- Diclofenac a potent NSAID often prescribed for severe joint pain, available as oral tablets and topical gels.
- Meloxicam a semi‑selective COX‑2 inhibitor that falls between traditional NSAIDs and pure COX‑2 blockers.
- Aspirin the original NSAID, primarily used for low‑dose cardiovascular protection but also for mild pain.
Side‑Effect Profiles: GI vs Cardiovascular Risks
Understanding the trade‑off between stomach safety and heart safety is key when picking an NSAID.
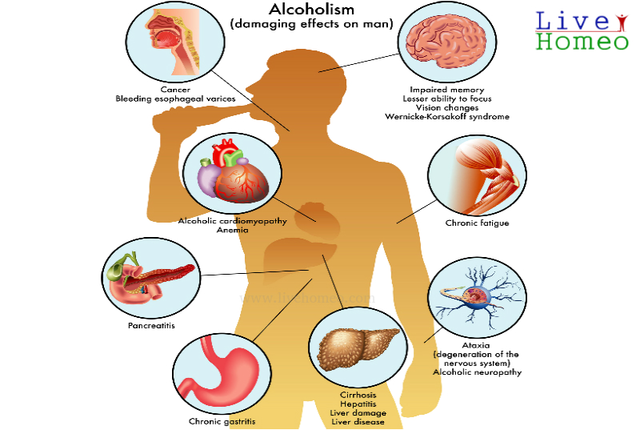
Non‑selective NSAIDs (ibuprofen, naproxen, diclofenac, aspirin) inhibit COX‑1, which can damage the stomach lining. Up to 20% of chronic users develop gastritis or ulcers, especially at higher doses.
COX‑2‑selective drugs like Celebrex and meloxicam reduce that GI risk but have been linked to a 1.5‑2% increase in serious cardiovascular events (heart attack or stroke) in large trials. Diclofenac also carries a higher CV risk despite being non‑selective.
Patients with a history of ulcers may benefit from Celebrex, while those with heart disease should discuss alternatives such as naproxen, which some data suggest has a more neutral CV profile.
Comparative Table
| Attribute | Celebrex (celecoxib) | Ibuprofen | Naproxen | Diclofenac | Meloxicam | Aspirin |
|---|---|---|---|---|---|---|
| COX Selectivity | COX‑2 selective | Non‑selective | Non‑selective | Non‑selective (higher COX‑2 affinity) | Partial COX‑2 selectivity | Non‑selective |
| Typical Dose for Osteoarthritis | 200mg once daily | 400-800mg three times daily | 250-500mg twice daily | 50mg two to three times daily | 7.5mg once daily (low) or 15mg once daily (high) | 81mg once daily (low‑dose) or 325mg up to 4× daily (pain) |
| Onset of Relief | 1-2hours | 30-60minutes | 60-90minutes | 30-60minutes | 2-3hours | 30-60minutes |
| GI Ulcer Risk | Low (≈2%) | Moderate‑High (≈10‑15%) | Moderate‑High (≈10‑12%) | High (≈12‑15%) | Low‑Moderate (≈5‑8%) | Low (≤2%) at low dose, higher at analgesic doses |
| Cardiovascular Risk | Increased (≈1.5‑2%) | Neutral‑to‑slight increase | Neutral (some studies suggest lower risk) | Increased (≈2‑3%) | Similar to Celebrex (moderate increase) | Low‑dose protective, high‑dose increases risk |
| Average Monthly Cost (US, 2025) | $70‑$90 (brand) / $30‑$45 (generic) | $10‑$20 (generic) | $15‑$25 (generic) | $25‑$40 (generic) | $35‑$55 (generic) | $5‑$12 (generic) |
When to Choose Celebrex
If you have a history of stomach ulcers or are taking blood thinners that increase bleeding risk, Celebrex’s lower GI profile can be a real advantage. It’s also convenient for people who prefer once‑daily dosing.
On the flip side, if you’ve had a heart attack, stroke, or uncontrolled hypertension, discuss alternatives with your doctor. Naproxen or low‑dose aspirin may be safer for heart health, while a proton‑pump inhibitor (PPI) can protect the stomach if you need a non‑selective NSAID.

Cost and Accessibility Considerations
In Australia, Celebrex is listed on the Pharmaceutical Benefits Scheme (PBS) for specific indications, which can bring the price down to about AU$15 per month for eligible patients. However, many private prescriptions still cost around AU$30‑$45.
Over‑the‑counter options like ibuprofen and naproxen are far cheaper and readily available in supermarkets and pharmacies. If budget is a primary concern, starting with a generic NSAID and adding a PPI for stomach protection can be a cost‑effective strategy.
Practical Tips for Safe Use
- Take the medication with food to reduce any mild stomach upset.
- Never exceed the recommended dose; higher doses don’t necessarily mean better pain relief but do raise risk.
- Check with your doctor before combining Celebrex with blood thinners, antihypertensives, or other NSAIDs.
- If you notice sudden chest pain, shortness of breath, or signs of a bleeding ulcer (dark stools, vomiting blood), seek medical help immediately.
- Regularly review the need for ongoing NSAID therapy with your healthcare provider-sometimes physical therapy or lifestyle changes can reduce reliance on medication.
Bottom Line
Choosing between Celebrex and other NSAIDs isn’t a one‑size‑fits‑all decision. Celebrex shines for people who need strong anti‑inflammatory power without the stomach irritation that comes with many OTC options. Yet that benefit comes with a modest increase in cardiovascular risk, which makes it less suitable for patients with existing heart disease.
By weighing your personal health history, pain severity, and budget, you can land on the drug that offers the best balance of relief and safety.
Frequently Asked Questions
Can I take Celebrex and ibuprofen together?
No. Combining a COX‑2 inhibitor with a non‑selective NSAID increases both GI and cardiovascular risks without providing extra pain relief. Talk to your doctor about alternative pain management strategies.
Is Celebrex safe for long‑term use?
Celebrex can be used long‑term for chronic arthritis if your doctor monitors your heart health and kidney function regularly. Routine blood tests every 3-6months are common practice.
How does the cost of Celebrex compare in Australia?
On the PBS, eligible patients pay around AU$15 per month. Without subsidy, the price climbs to AU$30‑$45. By contrast, generic ibuprofen typically costs less than AU$5 for a month’s supply.
What are the signs of a serious side effect from Celebrex?
Watch for chest pain, shortness of breath, sudden swelling of legs, dark or tarry stools, vomiting blood, or a sudden rash. Any of these symptoms warrant immediate medical attention.
Is meloxicam a good middle ground between Celebrex and ibuprofen?
Meloxicam offers partial COX‑2 selectivity, so it reduces GI risk more than ibuprofen but still carries a modest cardiovascular warning. It may suit patients who need once‑daily dosing but cannot take a pure COX‑2 inhibitor.





19 Comments
Wow, reading this guide felt like stepping into a medical drama; the way it lays out the GI vs CV trade‑off is sooo helpful, especially for us Canadians who love a good, safe pain reliever without breaking the bank.
I appreciate the clear tables and the note about the PBS in Australia – even though I'm north of the border, it shows how pricing varies worldwide.
The bit about taking it with food to ease mild stomach upset is a solid tip.
Overall, great balance of science and practical advice!
While the article attempts to be comprehensive, it suffers from a lack of nuanced pharmacological critique that a true connoisseur would expect.
The simplistic dichotomy of GI versus CV risk glosses over the complex interplay of COX isoforms and patient genetics.
Moreover, the cost comparison fails to account for insurance formularies that heavily influence actual out‑of‑pocket expenses.
The comparison chart reminds us that drug selection is rarely a binary choice, but rather a multidimensional optimization problem. When we consider the pharmacokinetic profiles, celecoxib’s once‑daily dosing offers adherence advantages over the three‑times‑daily regimen of ibuprofen. Yet, the modest increase in cardiovascular events reported for COX‑2 selective agents cannot be dismissed lightly, especially in patients with pre‑existing atherosclerotic disease. The gastrointestinal safety of celecoxib does present a compelling case for individuals with a history of ulcer disease who might otherwise be contraindicated to non‑selective NSAIDs. From an economic standpoint, the generic availability of celecoxib narrows the price gap, though brand‑only prescriptions still impose a significant financial burden on many. It is also worth noting that the onset of analgesia for ibuprofen and diclofenac, being within 30‑60 minutes, may be preferable for acute flare‑ups where rapid relief is desired. Conversely, the slower onset of celecoxib, taking up to two hours, aligns more with chronic management where peak plasma concentrations are less critical. The article’s brief mention of proton‑pump inhibitors as a gastroprotective strategy could be expanded, as PPIs have become a standard adjunct for high‑risk NSAID users. In clinical practice, shared decision‑making should incorporate patient values, such as tolerance for daily pill burden versus risk aversion. For patients with hypertension, the potential for COX‑2 inhibitors to elevate blood pressure adds another layer of complexity that warrants vigilant monitoring. The meta‑analyses cited in the literature suggest that naproxen may confer a modest cardioprotective effect, a nuance that could influence prescribing in cardiology‑focused settings. Meanwhile, aspirin’s dual role as an antiplatelet agent and analgesic underscores its unique position, though the gastrointestinal trade‑off at higher doses remains a concern. The table’s clear delineation of risk percentages aids in visualizing these trade‑offs, yet clinicians must remember that individual variability often deviates from population averages. Ultimately, the decision to select celecoxib over an alternative should emerge from a synthesis of pharmacodynamic properties, comorbid conditions, and socioeconomic factors. In sum, this guide serves as a valuable scaffold upon which personalized therapeutic plans can be built, provided we remain attentive to the subtleties it briefly touches upon.
Celebrex just isn’t worth the heart risk
From a pharmacoeconomic perspective, the incremental cost‑effectiveness ratio (ICER) of celecoxib versus generic ibuprofen hinges on the magnitude of avoided gastrointestinal events.
When the number needed to treat (NNT) to prevent one ulcer is high, the additional expense may not be justified for low‑risk patients.
Conversely, in a high‑risk ulcer cohort, the reduction in bleeding complications translates into tangible savings in hospitalisation costs.
Thus, tailoring therapy based on individual risk stratification maximizes both clinical outcomes and budgetary efficiency.
The article presents the data in a clear, concise manner, making it easy to compare each NSAID’s risk profile and cost.
Its inclusion of both brand and generic pricing helps readers gauge real‑world affordability.
Overall, a well‑structured resource for anyone weighing pain‑relief options.
Oh great, another “comprehensive” guide that pretends to be neutral while clearly favoring the pricey brand.
Because what we really needed was a chart that tells us to spend more money for the same effect.
Seriously, the author could have saved us all a lot of scrolling.
Thank you for the thorough overview; the balanced presentation of gastrointestinal and cardiovascular considerations is particularly valuable for clinicians.
I appreciate the emphasis on shared decision‑making and the practical tips regarding dosing and co‑medication.
Love how this broke down the stuff! 😍 Super helpful for my arthritis pain 🙌 Hope it saves me from a stomach ulcer 😅
This guide is a great start! 👍 It’s clear, friendly, and gives useful tips to keep costs down while staying safe.
Keep up the good work!
Interesting read, though the tone swings between formal analysis and sarcastic aside, making the takeaways a bit fuzzy.
Nevertheless, the risk tables are spot on.
Solid info, thanks.
Alright, let’s cut through the fluff – if you can tolerate a bit of stomach drama, ibuprofen gets you pain relief fast and cheap; if you’re scared of ulcers, celecoxib is the sleek, once‑daily hero, but watch that heart ticking like a time bomb.
Choose wisely.
Your enthusiasm for the comparative tool is contagious – I can already see it helping patients make smarter choices about pain management.
Wow, another “objective” comparison? Clearly the pharma lobby is pulling the strings!!! The data is cherry‑picked to push the most expensive brand while hiding the real dangers – don’t be fooled!!!
Great job simplifying a complex topic! Keep it up, and more people will feel confident choosing the right NSAID for their needs.
These tables are a trap – they hide the truth about how big pharma manipulates risk stats to keep us buying their “premium” pills. Stay vigilant!
Reading through this guide, I can’t help but feel a warm sense of reassurance that we’re not left to wander blindly in the wilderness of NSAID choices.
It’s like having a knowledgeable friend who patiently walks you through each option, pointing out the subtle differences in how each drug interacts with your body’s unique chemistry.
The clear breakdown of GI versus cardiovascular risk really shines a light on why one might favor celecoxib for a sensitive stomach, while still reminding us of the heart considerations that should not be ignored.
And the cost section? Absolutely essential, because what good is a perfect medication if it bankrupts you.
Overall, this is a solid, user‑friendly resource that bridges the gap between medical jargon and everyday decision‑making.
While the analysis is competent, it lacks the depth expected from a truly scholarly exposition on COX inhibition nuances.