Not every drug you pick up at the pharmacy has a cheaper generic version - and even when it does, it might not be the kind you think. There’s a hidden layer in the generic drug market called authorized generics, and they’re not available for most medications. If you’ve ever been confused why your "generic" pill suddenly looks different, or why some expensive drugs have a low-cost version while others don’t - this is why.
What Exactly Is an Authorized Generic?
An authorized generic is the exact same drug as the brand-name version, made by the same company, in the same factory, with the same ingredients and packaging - just sold under a different label and at a lower price. It’s not a copy. It’s the real thing, repackaged. The FDA lists these separately from traditional generics because they’re produced under the original brand’s New Drug Application (NDA), not a separate Abbreviated New Drug Application (ANDA).That means no waiting for bioequivalence studies. No delays. No legal battles. The brand company simply decides to make a version of their own drug and sell it as a generic. For example, when Mylan launched its authorized generic of the EpiPen in 2016, it was identical to the brand version - same epinephrine dose, same auto-injector mechanism, same manufacturing line. The only difference? The box said "EpiPen Authorized Generic" instead of "EpiPen."
Why Don’t All Drugs Have Authorized Generics?
The short answer: because brand companies choose not to make them.Authorized generics don’t happen by accident. They’re a business decision. Only about 1,215 authorized generics existed in the U.S. as of 2019 - out of thousands of brand-name drugs. That’s less than 10% of all prescription medications. Why so few?
Brand manufacturers only launch authorized generics when it helps them financially. They’re most common for high-revenue drugs - those making over $500 million a year. In fact, 89% of top-selling drugs ($1 billion+ in annual sales) have used authorized generics at some point. Meanwhile, only 22% of drugs under $100 million in sales ever had one.
Why? Because launching an authorized generic costs money. You need to repackage, relabel, set up distribution, and manage regulatory paperwork. If a drug only brings in $50 million a year, it’s not worth the effort. But if it’s a $2 billion drug like Lyrica or Protonix? Suddenly, the math changes.
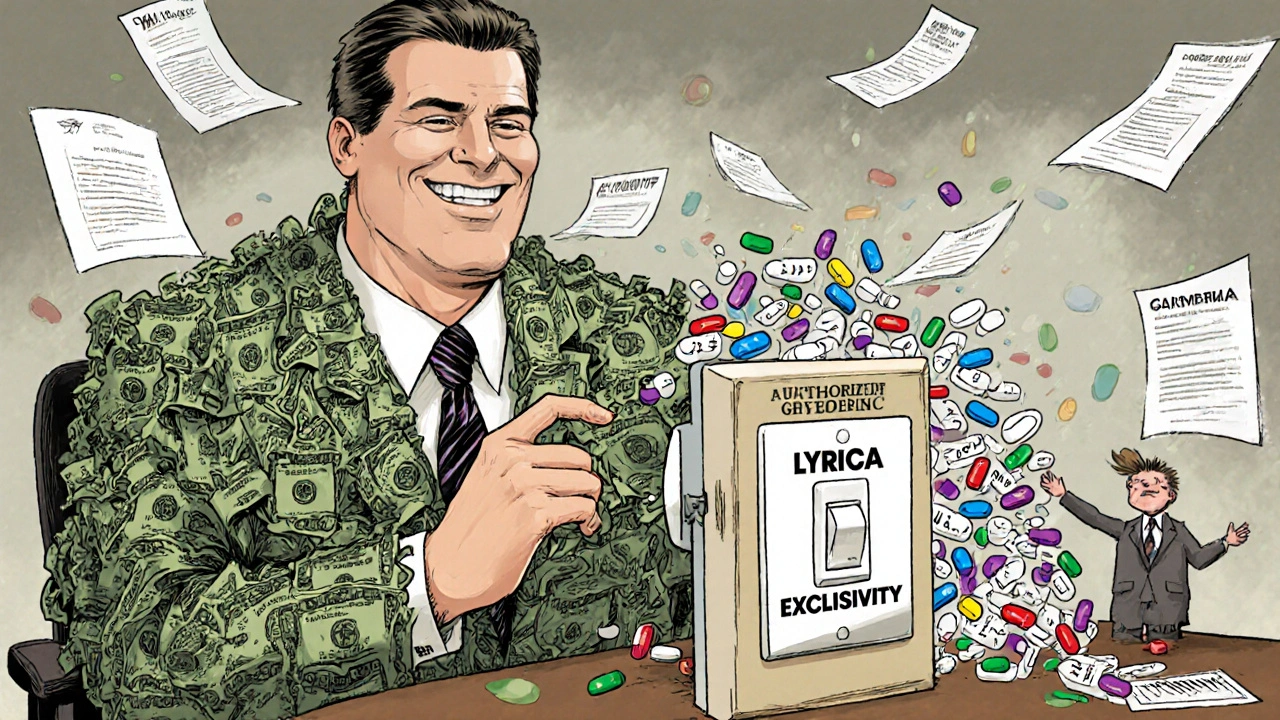
The Strategic Game Behind Authorized Generics
Authorized generics aren’t just about lowering prices - they’re about controlling competition.Under the Hatch-Waxman Act, the first company to file a generic version of a drug gets 180 days of exclusivity. During that time, no other generic can enter the market. That’s a huge financial advantage - potentially hundreds of millions in extra profit.
But here’s the twist: if the brand company launches its own authorized generic during that 180-day window, it splits the market. The first generic company still gets to sell, but now they’re competing with the exact same product at the same price. The FTC found this cuts the first generic’s revenue by 40-52% during exclusivity and up to 62% over the next 30 months.
For brand companies, this is a smart move. They keep market share. They prevent the generic from dominating. And they still make money - just less than before. In 2010, when Teva launched an authorized generic of Protonix, it priced it 35% below the brand version. That still left them with a profitable product, while shutting out other generic competitors.
Some brand companies even use authorized generics as a threat. They’ll negotiate with generic manufacturers to settle patent lawsuits - and in exchange for dropping their challenge, the brand promises not to launch an authorized generic. Stanford Law School found that 78% of patent settlements between 2018 and 2022 included these "no-AG" clauses, up from 62% in the previous five years.
Who Benefits - and Who Gets Left Out?
Consumers sometimes see lower prices when authorized generics enter the market. The FTC reported retail prices dropped 4-8% and wholesale prices fell 7-14% during the 180-day exclusivity window. AARP found patients saved an average of $18.75 per prescription when an authorized generic was available.But here’s the catch: those savings only happen if the brand company decides to launch one. For the other 90% of drugs? No authorized generic. No price drop. Just the brand-name price - or a traditional generic that might still be expensive because no one else is competing.
And it gets worse. Authorized generics can actually make it harder for other generic companies to enter the market. Why risk millions of dollars in legal fees and manufacturing costs if the brand company can just drop its own version and crush your profits? Harvard’s Aaron Kesselheim found this discourages generic challengers - especially for complex drugs where the cost to develop a traditional generic is high.
Confusion at the Pharmacy Counter
Authorized generics aren’t just a business tool - they’re a logistical headache.Pharmacists report more errors when both brand and authorized generic versions are available. Walgreens staff documented a 27% increase in prescription processing mistakes because the pills look identical, but the labels are different. Patients get confused too. One Medicare Part D survey found 72% of respondents didn’t understand why their "generic" suddenly came in a new box with a different name.
Doctors aren’t immune. A 2018 AMA survey of 1,200 physicians showed 63% found authorized generics made therapeutic substitution decisions harder. If a patient’s prescription says "generic" but the pharmacy gives them the brand’s own version, is that still the same? What if the patient had a reaction before? Who’s responsible?
What’s Changing - and What’s Not
The FDA started updating its authorized generic list quarterly in January 2022, after years of only releasing annual reports. That’s progress - but it doesn’t change the core problem: availability is still entirely up to the brand company.Congress has tried to fix this. The Preserve Access to Affordable Generics and Biosimilars Act has been reintroduced multiple times with bipartisan support. It would ban brand companies from launching authorized generics during the 180-day exclusivity period. But so far, it hasn’t passed.
The FTC is watching closely. In 2023, they filed legal briefs arguing that authorized generics undermine competition. Goldman Sachs predicts their use will decline by 15-20% over the next decade as biosimilars grow. But for now, they’re still a powerful tool in the brand drug playbook.
What This Means for You
If you’re paying for a brand-name drug and wondering why there’s no cheaper version - don’t assume the generic market has failed. It might just be that the brand company hasn’t chosen to let one in.Ask your pharmacist: "Is there an authorized generic for this?" If yes, you might get the same drug for less. If no, ask why. Sometimes, the answer is simple: the drug isn’t profitable enough to justify a generic version. Other times, the answer is more complex: the company is holding back competition to protect its profits.
There’s no magic fix. Authorized generics aren’t a solution to high drug prices - they’re a strategic maneuver within a broken system. The only way to ensure real, lasting price reductions is to have multiple independent generic manufacturers competing. But right now, that’s the exception - not the rule.
Until that changes, your best move is to know your options. Check the FDA’s authorized generic list. Talk to your pharmacist. Ask your doctor if a different drug in the same class might work. And remember: just because a drug doesn’t have a generic doesn’t mean it’s the only option - it just means the system isn’t working for you yet.
Are authorized generics the same as regular generics?
Yes and no. Authorized generics are physically identical to the brand-name drug - same ingredients, same factory, same quality control. They’re just sold under a different label. Regular generics are made by different companies and must prove they’re bioequivalent to the brand. Authorized generics skip that step because they’re made by the brand company itself.
Why don’t all brand-name drugs have authorized generics?
Because the brand company has to choose to make one. It’s a business decision. Authorized generics are only worth it for high-revenue drugs - usually those making over $500 million a year. For cheaper drugs, the cost of relabeling and distribution isn’t worth the small profit gain. Most drugs simply don’t have the financial incentive for a brand company to launch an authorized version.
Do authorized generics lower drug prices?
Sometimes - but only if they’re launched. When they enter the market during the 180-day exclusivity period for the first generic, they can reduce retail prices by 4-8% and wholesale prices by 7-14%. But if the brand company never launches one, prices stay high. That’s why many drugs still cost hundreds of dollars even after patents expire.
Can I ask my pharmacist for an authorized generic?
Yes, absolutely. Ask: "Is there an authorized generic version of this drug?" If one exists, they can usually fill your prescription with it. It’s the same drug, just cheaper. You might need to ask twice - some pharmacists aren’t trained to recognize the difference between authorized generics and regular generics.
Are authorized generics safe?
Yes. Since they’re made by the same company, in the same facility, with the same formula as the brand-name drug, they’re just as safe and effective. The FDA lists them separately for tracking, but there’s no difference in quality or performance. If your doctor prescribed the brand, the authorized generic is a direct substitute.
Why do some people say authorized generics hurt competition?
Because they’re a tool used by brand companies to block other generic manufacturers. When a brand launches its own generic during the 180-day exclusivity period, it takes market share from the first generic company - often driving them out of the market. This discourages other companies from challenging patents in the future, since they know the brand might just flood the market with its own version. The FTC and some lawmakers argue this undermines the whole point of the generic drug system.
How do I find out if a drug has an authorized generic?
Check the FDA’s official list of authorized generics, updated quarterly. You can search by brand name or active ingredient. Your pharmacist can also look it up - but they might need to check the FDA database directly, since not all pharmacy systems track authorized generics separately from regular generics.





14 Comments
Authorized generics are just another way pharma companies milk the system. They’re not helping consumers-they’re just outmaneuvering competitors while keeping prices high. If the brand makes the same pill, why isn’t it required to offer it at a discount? The FDA should mandate it.
It is imperative to recognize that the distinction between authorized generics and traditional generics lies not in efficacy or safety, but in regulatory classification and corporate strategy. The FDA's separate tracking mechanism serves a vital purpose in pharmacovigilance and market transparency. Consumers should be empowered with accurate information to make informed decisions regarding their prescriptions.
It’s fascinating how capitalism turns healthcare into a chess game where the only winners are the ones who own the board. The authorized generic isn’t a solution-it’s a performance. We’re not fixing the system; we’re just dressing up its flaws in a different suit.
Let’s be real-this isn’t about competition. It’s about patent trolling disguised as market strategy. The 180-day exclusivity loophole? That’s corporate welfare with a pharmacy label. And don’t get me started on the ‘no-AG’ clauses. That’s collusion with a white coat.
So basically, if you’re lucky, your drug might be cheaper. If not, you’re screwed. Thanks, Big Pharma.
Think about it-this isn’t just economics, it’s psychology. The brand company knows you trust the name. They know you’ll pay more for the same pill if it’s in a familiar box. So they give you the same pill in a cheaper box… but only if it’s profitable. And then they punish anyone who tries to compete by flooding the market with their own version. It’s emotional manipulation wrapped in regulatory language. We’ve turned medicine into a hostage situation where the drug is the hostage and the patient is the ransom payer. And the worst part? We’ve been conditioned to accept it as normal. We don’t question why the same pill costs $100 one day and $20 the next. We just take it. Literally and figuratively. We’ve lost the ability to demand fairness because we’ve been taught that ‘market forces’ are sacred. But markets don’t care about sick people. Only profits do. And until we stop treating healthcare like a stock ticker, we’ll keep losing.
There’s something deeply ironic about this whole system. We’re told generics are the answer to high drug prices, but the real power lies in who gets to define what a generic even is. The brand company holds the keys to the pharmacy-and they’re not handing them out. It’s like saying you can buy the same car as a luxury model, but only if the manufacturer decides to make a budget version. And even then, they’ll make sure no one else can build a better one. The whole thing feels less like a market and more like a monopoly with a side of theater. We’re not fighting for cheaper drugs-we’re fighting for the right to have choices that aren’t controlled by the same people who made the prices sky-high in the first place.
Oh wow, so the drug company just… made a cheaper version of their own drug? Shocking. Next they’ll tell us they’re donating to hospitals. Look, I get it-you’re proud you didn’t have to pay $500 for your EpiPen. But let’s not pretend this is altruism. This is a tactical retreat. A feint. A way to keep the real generics out while still collecting cash. If this was truly about lowering prices, we’d have 10 companies making the same pill. But we don’t. We have one company making two versions of the same pill… and calling it ‘choice.’ Thanks, but I’ll take real competition over corporate theater any day.
This is a very thoughtful analysis. In my country, we have strict price controls, so authorized generics are not common. But I see the logic-when a company chooses to offer a lower-priced version, it can help patients. Still, the system should ensure that competition is fair. Perhaps government incentives could encourage more authorized generics for mid-tier drugs, not just the billion-dollar ones. Everyone deserves access, not just those with expensive prescriptions.
One thing people overlook: pharmacists are often the first line of defense here. If your pharmacist doesn’t know what an authorized generic is, you’re not getting the full benefit. Ask for it by name. Know your active ingredient. And if they say ‘no generic available,’ ask: ‘Is there an authorized generic?’ That simple question can save you hundreds. Don’t let ignorance at the counter cost you money.
Stop pretending this is about patient care. This is about profit maximization wrapped in a lab coat. The fact that companies are allowed to block competitors by launching their own generics? That’s not innovation-that’s extortion. And the FDA? They’re watching. Watching while the system burns. We need to break the patent system open, not polish its edges. This isn’t a fix-it’s a bandage on a hemorrhage.
It’s amazing how something so simple-like a pill in a different box-can reveal so much about our system. I wish more people knew this. I’ve seen friends pay full price for years because they didn’t know the authorized generic existed. Maybe we need public awareness campaigns. Not ads for drugs, but ads for knowledge. ‘Your pill might be cheaper. Ask your pharmacist.’ Simple. Powerful.
Let me tell you what’s really happening. This isn’t about generics. It’s about control. The pharmaceutical giants, the FDA, the insurance companies-they’re all in bed together. The authorized generic? A distraction. A smokescreen. They want you to think the system is working because you got a ‘cheaper’ version. But it’s still their drug. Still their factory. Still their price. And if you think the FTC is going to stop them, you’re dreaming. They’re the ones who approved the system in the first place. This is all a carefully orchestrated illusion. They’re not trying to lower prices-they’re trying to make you feel like you’re getting a deal while they keep the real money. Wake up.
Love this breakdown. Honestly, it’s wild how something as small as a label change can expose such a broken system. I’ve had my own experience-switched to an authorized generic for my blood pressure med and saved $120/month. No side effects, no fuss. But I had to dig for it. Shouldn’t have to be a detective just to get a fair price. Maybe we need a simple ‘Authorized Generic Available’ sticker on the shelf? Little things like that could make a huge difference.