Think your meds are safe just because your doctor prescribed them? Think again. Many people don’t realize that drug-disease interactions can turn a life-saving pill into a dangerous one - not because of what else you’re taking, but because of what’s already wrong with your body.
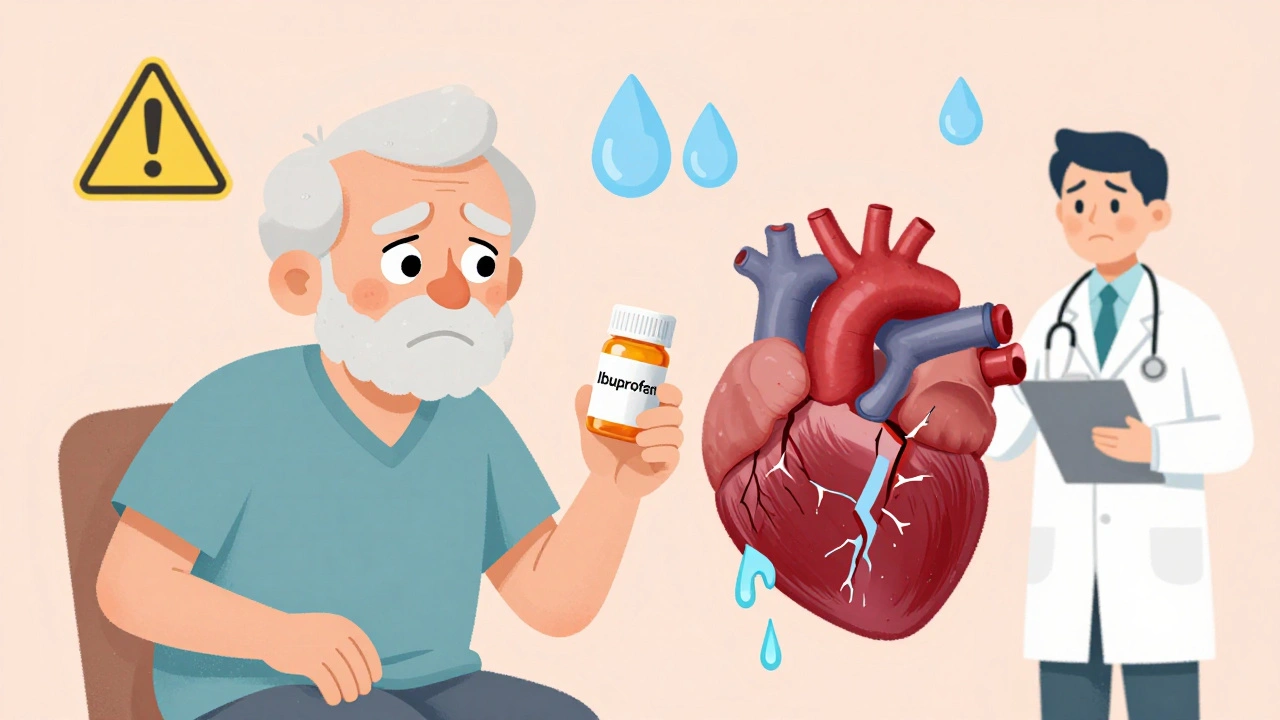
Take someone with heart failure who gets prescribed an NSAID like ibuprofen for arthritis pain. Sounds harmless, right? But that same drug causes your body to hold onto salt and water, making heart failure worse. Or a diabetic on beta-blockers for high blood pressure - those meds can hide the warning signs of low blood sugar, like shaking or sweating, so the person doesn’t know they’re in danger until it’s too late.
These aren’t rare edge cases. They happen every day. The Agency for Healthcare Research and Quality estimates that 5 to 10% of hospital admissions are caused by medication problems, and a big chunk of those come from drug-disease interactions. Yet most patients, and even many doctors, don’t think to ask: Does my condition make this drug riskier?
How Your Body Changes How Drugs Work
Drugs don’t work the same way in every body. When you have another illness, your body’s chemistry shifts - and that changes how medications are absorbed, processed, or even how they affect your organs.
There are five main ways this happens:
- Pharmacodynamic interference: The drug fights against your disease. For example, beta-blockers slow your heart rate - great for high blood pressure - but they can tighten airways and make asthma attacks worse.
- Pharmacokinetic changes: Your disease messes with how your liver or kidneys break down the drug. If you have liver disease, warfarin (a blood thinner) stays in your system longer, raising your risk of dangerous bleeding.
- Masking symptoms: Some drugs hide the signs of another condition. Beta-blockers in diabetics can hide the tremors and sweating that tell you your blood sugar is dropping.
- Exacerbating complications: Drugs can make existing problems worse. NSAIDs cause fluid retention, which is fine for healthy people but can trigger sudden heart failure in someone with weakened heart muscle.
- Direct organ toxicity: Some drugs are safe for healthy kidneys but deadly for damaged ones. Metformin, a common diabetes drug, can cause lactic acidosis if your kidneys aren’t filtering properly.
These aren’t theoretical risks. A 2015 study found that 84% of serious drug-disease interactions in diabetes patients involved kidney disease. Another analysis showed that 42% of risks in depression treatment came from bleeding - mostly from SSRIs interacting with conditions like ulcers or clotting disorders.
The Top Four Conditions That Cause the Most Problems
Not all diseases create the same level of risk. Four conditions stand out as major drivers of dangerous drug-disease interactions:
- Chronic kidney disease: Over half of all high-risk interactions involve drugs cleared by the kidneys. Metformin, lithium, and certain antibiotics can build up to toxic levels if kidney function drops.
- Heart failure: Fluid-retaining drugs like NSAIDs, calcium channel blockers, and even some diabetes meds can worsen swelling and shortness of breath.
- Liver disease: The liver breaks down most medications. If it’s damaged, drugs like statins, benzodiazepines, and warfarin stick around too long, increasing side effects.
- Psychiatric conditions: Depression, bipolar disorder, and schizophrenia often require multiple medications that interact with each other and with physical illnesses. SSRIs can cause bleeding in people with ulcers or on blood thinners. Lithium becomes toxic if kidney function declines or dehydration occurs.
These four conditions account for nearly 80% of documented serious drug-disease interactions, according to the American Society of Health-System Pharmacists. And the risk goes up the more conditions you have.
Why This Is Often Overlooked
You’d think doctors would be trained to spot these. But here’s the problem: most clinical guidelines focus on treating one disease at a time.
A 2015 study looked at guidelines for diabetes, depression, and heart failure. Only 16% of them mentioned drug-disease interactions. That means if you’re a diabetic with kidney disease, your doctor might follow the diabetes guidelines - and miss that metformin is now unsafe for you.
Electronic health records (EHRs) are supposed to help. Epic’s system flags 87% of high-risk interactions - but 42% of those are false alarms. Doctors start ignoring them. It’s called alert fatigue. By the time a real danger pops up, the system is ignored.
Even pharmacists struggle. A 2021 survey found community pharmacists spend nearly 13 minutes per patient checking for these interactions - but most don’t have that kind of time during a routine refill. Patients rarely bring up their full list of conditions. They mention diabetes. They forget about the mild kidney issue. Or the heart rhythm problem their cardiologist told them to ignore.

Who’s Most at Risk?
Older adults are the most vulnerable. The average person over 65 takes 5.4 medications and has 4.7 chronic conditions. That’s a perfect storm for interactions.
The FDA points out that seniors are especially at risk because their kidneys and liver don’t process drugs as well. A drug that’s safe for a 40-year-old might be dangerous for a 75-year-old with the same diagnosis.
But it’s not just age. People in marginalized communities face 23% higher rates of drug-disease related hospitalizations, according to Health Affairs (2023). Why? Fragmented care. No primary doctor. Poor communication between specialists. Medication lists that don’t get updated.
And then there are supplements. St. John’s wort, often taken for low mood, can cause serotonin syndrome when mixed with SSRIs - a potentially fatal reaction. Many people think “natural” means “safe.” It doesn’t.
What You Can Do to Stay Safe
You don’t have to wait for your doctor to catch this. Here’s how to protect yourself:
- Keep a full, updated list of everything you take: Not just prescriptions. Include over-the-counter drugs, vitamins, herbs, and supplements. Write down the dose and why you take it.
- Ask: “Could this drug make any of my other conditions worse?” Don’t assume your doctor knows. If you have kidney disease, ask about metformin. If you have asthma, ask about beta-blockers. If you’re on blood thinners, ask about NSAIDs.
- Use the Beers Criteria: This is a list of potentially unsafe drugs for older adults, updated yearly by the American Geriatrics Society. You can look it up online. It includes warnings like “avoid anticholinergics in dementia” or “avoid opioids in COPD.”
- Get regular kidney and liver tests: If you’re on long-term meds, ask for blood work every 6-12 months. A simple creatinine test can show if your kidneys are struggling.
- Use one pharmacy: If all your prescriptions go through one pharmacy, they can run interaction checks across your entire list. Chain pharmacies have better systems than small ones.
The Specialist Pharmacy Service recommends the DUP-OP-ALT framework: look for Duplication (two drugs doing the same thing), Opposition (drugs working against each other), and Alteration (drugs changing how your body handles another drug). It’s simple. It works.
The Future: Smarter Screening
Change is coming - slowly. The FDA now requires drug makers to test their products in patients with common comorbidities. New drugs must show how they behave in people with kidney or liver disease.
The NIH’s All of Us program is building a database that links your genes, your health history, and your meds to predict your personal risk. Early results show 38% better accuracy than old methods.
Machine learning tools are being tested at universities like Toronto. One system analyzed 157 clinical factors - from age to lab values to diagnosis codes - and predicted dangerous interactions with 89% accuracy. That’s better than any human.
But tech alone won’t fix this. The real fix is awareness. Patients need to speak up. Doctors need to ask better questions. Guidelines need to include comorbidities - not just single diseases.
By 2030, the Institute for Safe Medication Practices estimates that better screening could prevent 120,000 hospitalizations in the U.S. alone. That’s not a number. That’s 120,000 people who don’t end up in the ER because their blood pressure med made their kidney failure worse.
Final Thought: Your Body Is Not a Checklist
Medicine treats diseases like separate boxes. But your body doesn’t work that way. If you have three conditions, you don’t get three separate treatments. You get one complex system - and drugs interact with all of it.
Don’t let a single prescription become a hidden threat. Ask the questions. Know your conditions. Know your meds. And don’t assume safety just because it’s on paper.
Can a drug-disease interaction happen even if I’m not taking multiple medications?
Yes. Even a single medication can be dangerous if you have an underlying condition. For example, metformin is safe for most people with diabetes, but if you have kidney disease, it can cause lactic acidosis - a life-threatening buildup of acid in your blood. You don’t need to be on five drugs to be at risk. One drug plus one hidden condition is enough.
Are over-the-counter drugs safe if I have chronic conditions?
Not always. Common OTC drugs like ibuprofen, naproxen, and pseudoephedrine can worsen heart failure, high blood pressure, or kidney disease. Even antacids with magnesium or aluminum can be risky if you have kidney problems. Always check with your pharmacist before taking anything - even aspirin or cold medicine - if you have a chronic illness.
Why don’t doctors always warn me about these interactions?
Many doctors focus on treating the main condition they’re seeing you for. If you’re there for high blood pressure, they might not think to ask about your mild kidney issue or your history of asthma. Also, many clinical guidelines don’t include warnings about drug-disease interactions. It’s not negligence - it’s a system gap. That’s why it’s up to you to speak up and share your full health history.
How do I know if a drug is making my condition worse?
Watch for new or worsening symptoms after starting a new drug. If you’ve had heart failure for years and suddenly feel more swollen or short of breath after starting a new painkiller, that’s a red flag. If you’re diabetic and notice your blood sugar is dropping without warning signs, your beta-blocker might be masking it. Don’t wait. Call your doctor. Track your symptoms in a notebook - it helps them see the pattern.
Can I stop a medication if I think it’s causing a problem?
Never stop a prescribed medication on your own - even if you think it’s causing harm. Some drugs, like blood pressure or seizure meds, can cause serious rebound effects if stopped suddenly. Instead, write down your concerns, note when symptoms started, and schedule a visit with your doctor or pharmacist. They can help you safely adjust or switch to a better option.





12 Comments
I never realized how many of my meds could be quietly sabotaging my kidney function. I’ve got diabetes and mild CKD, and my doctor just kept prescribing metformin like it was harmless candy. I only found out the risk after reading this. Now I’m asking for alternatives. Why isn’t this common knowledge?
It is an incontrovertible fact that the modern medical paradigm exhibits a systemic failure in its approach to polypharmacy and comorbidity management. The reductionist model of disease classification, rooted in 19th-century pathology, is wholly inadequate for the complex, interconnected physiological landscapes of contemporary patients. This article, while commendable in its exposition, fails to address the institutional inertia perpetuated by pharmaceutical lobbying and guideline committees that remain siloed in disease-specific orthodoxy.
so like… if your liver is tired, your meds just kinda… sit there? like a guest who won’t leave? that’s wild. i never thought about it like that. i take a statin and i have fatty liver and i just assumed it was fine. guess i’m calling my doc tomorrow.
This is a critical insight that must be communicated to every patient, especially in developing nations where access to specialized care is limited. I urge healthcare providers to adopt the DUP-OP-ALT framework as a mandatory checklist during every medication review. Awareness saves lives.
They’re hiding this from us. Big Pharma doesn’t want you to know your own body can turn your medicine into poison. They profit off hospitalizations. Your ‘safe’ prescription? It’s a trap. The FDA? Complicit. Your doctor? Just following the script.
Okay but what if you’re just healthy and take ibuprofen for headaches? Are we all just one kidney test away from being a walking medical disaster? This feels like fear-mongering dressed up as advice.
Metformin bad for kidneys. NSAIDs bad for heart. Beta blockers hide hypoglycemia. That’s it. You’re welcome.
we treat diseases like they’re separate apps on a phone but your body is one messy desktop with 47 tabs open and half of them crashing
USA has the best doctors and the worst system. Other countries don’t have this problem because they don’t let corporations run medicine. This is what happens when you privatize healthcare. You get death by paperwork and profit.
Really appreciate this breakdown. I’ve been managing type 2 diabetes and hypertension for over a decade, and I never connected the dots between my beta-blocker and the sudden episodes of unexplained fatigue and confusion. I thought it was just aging. Turns out, my body was screaming and I was too busy listening to the clock. I’ve since switched to an ARB and my blood sugar stability has improved dramatically. The key is tracking symptoms over time-not just numbers on a screen. Also, using one pharmacy was the best decision I ever made. They caught a dangerous interaction between my thyroid med and a common antacid I was taking for heartburn. No one else would’ve noticed.
my grandma took 12 pills a day and never asked a single question. she’s fine. maybe we’re overthinking this?
There’s a quiet revolution happening in pharmacogenomics and AI-driven clinical decision support. I’ve seen it firsthand-hospitals using machine learning models that analyze EHR data in real time to flag interactions even when the patient doesn’t mention their St. John’s wort or their ‘occasional’ NSAID use. It’s not perfect, but it’s changing outcomes. The real barrier isn’t tech-it’s time. Doctors are drowning. We need better systems, not just more patient education. This article nails the problem. Now let’s fix the pipeline.