There’s no such thing as a "generic vaccine" in the way there’s a generic version of aspirin or metformin. That’s not a technicality-it’s a fundamental barrier to global health equity. Unlike small-molecule drugs, vaccines are living products. They’re made from viruses, bacteria, or genetic material grown in cell cultures, purified, stabilized, and packaged under conditions so precise that even a tiny variation can ruin a batch. This isn’t chemistry. It’s biology on an industrial scale. And that’s why, despite decades of progress in generic drug production, billions of people still wait months-or years-for vaccines they need.
Why vaccines can’t be copied like pills
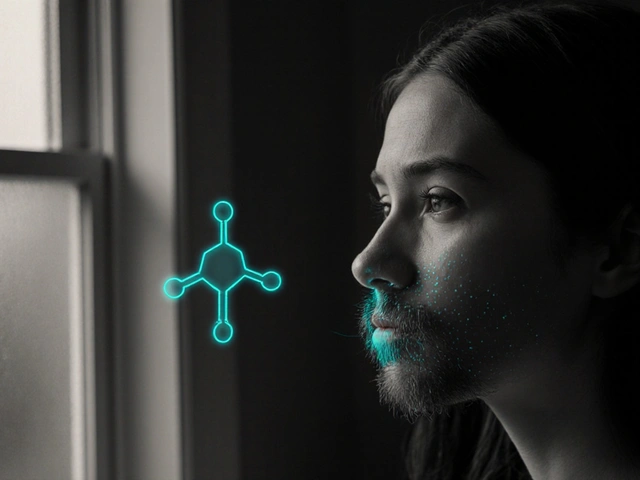
Generic drugs are copies. They use the same active ingredient, in the same dose, with the same effect. The FDA lets manufacturers prove they’re equivalent through lab tests and bioavailability studies. No need to repeat clinical trials. That’s the Hatch-Waxman Act, and it’s been working since 1984. But vaccines? They’re not chemical compounds. They’re complex biologicals. You can’t just dissolve them in water and test if they behave the same. Their structure, their purity, their stability-all matter. A single change in the cell line used to grow the virus, or a shift in temperature during purification, can alter how the immune system responds. That’s why every vaccine, even if it’s based on the same antigen, needs a full new license. No shortcuts. No abbreviated applications.The manufacturing wall
Building a vaccine factory isn’t like setting up a pill生产线. It takes $200 million to $500 million. It takes five to seven years. You need biosafety level 2 or 3 labs. You need ultra-cold freezers for mRNA vaccines-down to -70°C. You need specialized raw materials: lipid nanoparticles, cell substrates, growth media, adjuvants. Only five or seven companies in the world make the critical lipids used in mRNA vaccines. If one shuts down, supply chains crack. During the pandemic, India’s export ban on vaccine ingredients in April 2021 caused a global production drop of nearly 50%. That wasn’t politics. That was physics. No one else had the materials.Who makes the world’s vaccines?
India produces 60% of the world’s vaccines by volume. The Serum Institute of India alone can churn out 1.5 billion doses a year. It’s the largest vaccine maker on Earth. But here’s the twist: India imports 70% of its vaccine raw materials from China. That’s not independence. That’s vulnerability. Meanwhile, the top five companies-GSK, Merck, Sanofi, Pfizer, and Johnson & Johnson-control 70% of the global vaccine market. They set the prices. They control the supply. And they don’t have to compete on cost. In 2022, Gavi, the global vaccine alliance, still paid over $10 per dose for pneumococcal vaccine in low-income countries-even though the same vaccine cost less than $2 in some high-income markets. There’s no race to the bottom here. No generic price collapse. Just a take-it-or-leave-it model.
Where the gaps are
Africa produces less than 2% of its own vaccines. It imports 99%. During the pandemic, 83% of the 1.1 million COVID-19 doses delivered to Africa through COVAX went to just 10 countries. Twenty-three African nations vaccinated less than 2% of their populations. Health workers in the Democratic Republic of Congo got doses that would expire in two weeks-because there was no cold chain to store them. Meanwhile, the WHO’s mRNA technology transfer hub in South Africa, launched in 2021 with help from BioNTech, didn’t produce its first batch until September 2023. And even then, it’s only capable of 100 million doses a year. That’s less than 1% of global demand. The African Union estimates it will take $4 billion and 10 years just to get to 60% self-sufficiency by 2040. That’s not progress. That’s a delay.The false promise of technology transfer
The idea that you can just hand over the recipe and someone else will build it is a myth. The WHO’s hub in South Africa had access to the exact mRNA sequence, the protocols, the training. Still, it took 18 months just to get the equipment. Why? Because the machines that mix lipid nanoparticles don’t come from Amazon. They’re custom-built, single-source, and often controlled by Western suppliers. Export restrictions on those machines? They exist. And they’re not always public. When India faced its second wave, U.S. export controls on critical raw materials slowed global production. That’s not negligence. That’s policy. The same companies that own the patents also own the supply chains. And they’re not incentivized to break them.






15 Comments
Look i get it vaccines are complex but come on we’ve been doing this for decades. The real issue isn’t biology it’s corporate greed wrapped in a lab coat. Pfizer made 37 billion and still cried poverty. Meanwhile kids in Malawi are getting doses that expired last month. This isn’t science. It’s capitalism with syringes.
generic vaccine my ass. we all know it’s just a fancy way to say ‘let’s not make stuff here’
India makes 60% of the world’s vaccines but imports 70% of its raw materials from China. So we’re not independent we’re just a very large middleman with better packaging. The real joke? We’re the ones getting blamed when supply chains break. Meanwhile the real gatekeepers sit in Zurich and New Jersey sipping lattes and patenting lipids.
wait so if its not a generic like asprin then why do they call it the same thing? like isnt that misleading? also why do we even have this conversation like can we just make more factories? why is this so hard??
The entire paradigm of pharmaceutical sovereignty is a neoliberal illusion built on the corpse of public health. We’ve outsourced biological autonomy to a cartel of venture-capitalized biotech oligarchs who weaponize intellectual property as a tool of structural violence. The mRNA hub in South Africa isn’t failing because of technical limitations-it’s failing because the architecture of global capital refuses to decentralize the means of biological production. This isn’t about lipids or cold chains. It’s about who controls life itself.
you know what i think? we need to stop talking about patents and start talking about people. if a kid in the DRC gets a vaccine that expires in two weeks because there’s no fridge? that’s not a logistics problem. that’s a moral one. and we all know it.
It's important to recognize that while the technical barriers to vaccine production are immense, the moral ones are even greater. The fact that we can manufacture billions of doses yet still leave entire continents behind speaks less to scientific limitation and more to systemic neglect. India's Serum Institute is proof that low-cost, high-volume production is possible-but only when supported by global cooperation, not corporate monopolies. The path forward isn't about copying formulas; it's about sharing infrastructure, training, and equity.
you think this is about vaccines? no. this is about the deep state. the WHO and Gates foundation are pushing this so they can implant microchips through the needles. you think the cold chain is hard? try tracking where the lipid nanoparticles really come from. they’re not from China. they’re from DARPA. and the machines? made by a company owned by the same people who run the FDA. coincidence? i think not.
we have the tools. we have the knowledge. what we’re missing is the will. this isn’t a science problem. it’s a human one. if we cared as much about a child in Lagos as we do about a shareholder in Pfizer, we’d have 50 new vaccine factories by now. instead we’re still debating whether a generic is ‘technically’ possible. stop talking. start building.
why do people keep acting like this is a new problem? the same companies that made the vaccines owned the supply chains before the pandemic. they’ve always controlled the raw materials. they’ve always priced them like luxury handbags. the only thing that changed is we finally noticed. and now we’re mad? get over it. the system was designed this way. you want change? stop buying into the myth that transparency will fix it. it won’t. only disruption will.
I’ve worked in public health for 20 years and let me tell you-this isn’t about patents. It’s about trust. When a country sees its own health system being held hostage by foreign suppliers and pricing games, they don’t just feel powerless-they feel betrayed. That’s why local production isn’t just about efficiency. It’s about dignity. And dignity can’t be imported. It has to be built. Slowly. With help. But with real partnership-not charity.
so like… if the vaccine is so complex how come they made it in like 10 months?? 😅 like… if it’s so hard then why did it work so fast?? 🤔 maybe the whole thing is just a distraction??
One thing people miss: the real bottleneck isn’t the science or the patents-it’s the skilled labor. You can’t just build a factory and hire anyone. You need people trained in sterile processing, cryogenic logistics, quality control for biologicals. That takes years. And no one’s investing in that training outside the big players. We need global apprenticeship programs-not just tech transfer. Skills, not just schematics.
you think India is a vaccine powerhouse? lol. they make 60% of volume but 90% of it is for export. their own population still gets leftovers. and they’re importing key ingredients from China. so who’s really in control? the guy in Pune or the guy in Shanghai? this isn’t sovereignty. it’s outsourcing with a flag on the box
and that’s why we need real sovereignty not just assembly lines. if you’re importing your lipids from China and your cold chain tech from Germany and your QC software from Boston then you’re not independent-you’re just a very expensive contract manufacturer with a national anthem. the real power isn’t in the vial. it’s in the supply chain. and right now? we’re all just renting it.