Introduction to Bacterial Meningitis and Ampicillin
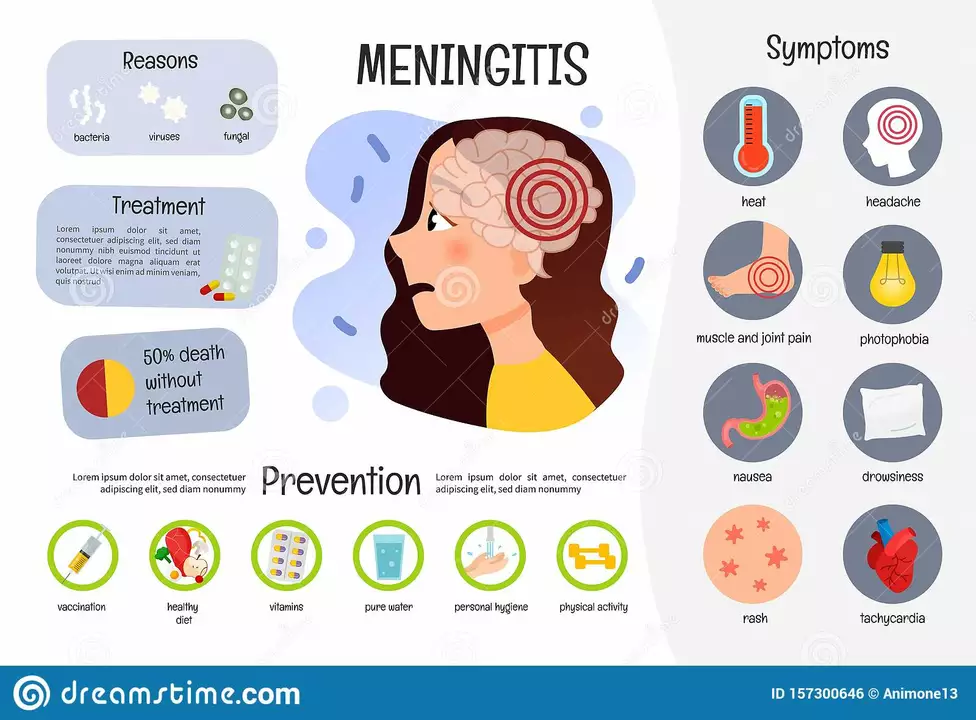
Bacterial meningitis is a severe infection that occurs when bacteria invade the membranes surrounding the brain and spinal cord. This can lead to dangerous inflammation and can cause numerous complications, including hearing loss, brain damage, and even death. Among the different antibiotics used to treat bacterial meningitis, ampicillin is one of the most commonly prescribed medications. In this article, we will discuss the use of ampicillin in treating bacterial meningitis, its effectiveness, and necessary precautions.
How Ampicillin Works Against Bacterial Meningitis
Ampicillin is a part of the penicillin family of antibiotics. It works by inhibiting the synthesis of bacterial cell walls, which ultimately leads to the death of the bacteria. As bacterial meningitis is caused by bacteria, ampicillin is effective in treating the infection by targeting the bacteria responsible for the illness. Ampicillin is particularly effective against gram-positive bacteria like Streptococcus pneumoniae and Listeria monocytogenes, which are common causes of bacterial meningitis.
Ampicillin Treatment Regimen
When it comes to treating bacterial meningitis with ampicillin, the dosage and length of treatment are crucial factors. Normally, a high dose of ampicillin is administered intravenously to ensure that the antibiotic reaches the central nervous system quickly and in sufficient amounts. The typical treatment regimen involves administering ampicillin every 4 to 6 hours for a duration of 10 to 14 days, depending on the severity of the infection and the patient's response to the treatment.
Combining Ampicillin with Other Antibiotics
One important aspect to consider when treating bacterial meningitis with ampicillin is that it may be more effective when used in combination with other antibiotics. For instance, ampicillin is often used alongside aminoglycoside antibiotics, such as gentamicin, to provide a broader spectrum of coverage against various types of bacteria. Combining ampicillin with other antibiotics can also help prevent the development of antibiotic-resistant bacteria, which is a growing concern in the field of medicine.
Side Effects and Precautions
While ampicillin is generally considered safe and effective for treating bacterial meningitis, it's essential to be aware of potential side effects and precautions. Some common side effects of ampicillin include diarrhea, nausea, vomiting, and rash. In rare cases, severe allergic reactions may occur, causing symptoms such as difficulty breathing, hives, and swelling of the face or throat. If you experience any signs of an allergic reaction, it is crucial to seek medical attention immediately.
It's also important to inform your healthcare provider of any other medications you are taking or if you have a history of allergies to penicillin or other antibiotics. Pregnant or breastfeeding women should consult their doctor before taking ampicillin, as it can pass through breast milk and may affect the baby.
Monitoring Treatment Progress
During the course of ampicillin treatment for bacterial meningitis, it is essential to monitor the patient's progress closely. Regular blood tests and spinal fluid analysis may be conducted to ensure the infection is clearing up and the antibiotic is effectively eliminating the bacteria. Your healthcare provider may also adjust the dosage or length of treatment as needed, based on your response to the medication.
Preventing Bacterial Meningitis
While ampicillin is effective in treating bacterial meningitis, the best approach is always prevention. Practicing good hygiene, such as washing hands regularly and avoiding close contact with sick individuals, can help reduce the risk of contracting bacterial meningitis. Additionally, there are vaccinations available to protect against some of the most common types of bacteria that cause meningitis, including Streptococcus pneumoniae, Neisseria meningitidis, and Haemophilus influenzae type b. Talk to your healthcare provider about the appropriate vaccinations for you and your family.





17 Comments
Ampicillin, when administered intravenously, achieves cerebrospinal fluid concentrations, essential for bacterial eradication; the dosing schedule, typically every 4 to 6 hours, aligns with pharmacokinetic targets, ensuring therapeutic levels; clinicians must monitor renal function, adjust dosage accordingly, and remain vigilant for adverse reactions.
I'm really glad you shared this-ampicillin can be a lifesaver, especially when paired with careful monitoring. 😊
Just remember to keep an eye on any side effects and stay in touch with your doctor.
Balancing effectiveness with safety is key; the guidelines you outlined make sense, and the emphasis on combination therapy reflects current practice.
I cant beleive ppl still overlook how ampicillin can be a double edged sword, especially in neonates! The risk of resistance is real, and the side effects can be harsh.
The therapeutic use of ampicillin in bacterial meningitis demands strict adherence to evidenced-based protocols; any deviation constitutes a dereliction of medical responsibility. First, the dosage must be calibrated to achieve cerebrospinal fluid concentrations that exceed the minimum inhibitory concentration for the targeted pathogens. Second, the timing of administration, typically every four to six hours, is non‑negotiable if we are to maintain bactericidal activity. Third, clinicians must obtain baseline renal and hepatic panels before initiating therapy, for ampicillin clearance is heavily dependent on organ function. Fourth, patients with a known penicillin allergy should be excluded without exception, as cross‑reactivity poses a severe, potentially fatal risk. Fifth, continuous monitoring of serum drug levels is advisable in cases of renal impairment to avoid toxicity. Sixth, adjunctive therapies, such as aminoglycosides, should be considered only when the microbial spectrum justifies broadened coverage. Seventh, the duration of treatment must be limited to the shortest effective interval, usually ten to fourteen days, to curb the emergence of resistant strains. Eighth, any manifestation of rash, gastrointestinal upset, or anaphylaxis warrants immediate discontinuation of the drug. Ninth, clinicians should educate patients and families about the signs of adverse reactions and the importance of adherence. Tenth, failure to observe these standards not only jeopardizes individual outcomes but also undermines public health efforts against antimicrobial resistance. Eleventh, the literature unequivocally supports the superiority of a regimented approach over empirical improvisation. Twelfth, institutional protocols should be updated regularly to reflect the latest consensus guidelines. Thirteenth, interdisciplinary collaboration between infectious disease specialists, pharmacists, and neurologists enhances therapeutic precision. Fourteenth, documentation of all dosing adjustments and patient responses is essential for medico‑legal accountability. Finally, any practitioner who neglects these imperatives is acting with reckless complacency, and such conduct must be subject to professional scrutiny.
The pharmacokinetic parameters of ampicillin, notably its volume of distribution and clearance rate, necessitate a high‑frequency IV infusion to sustain optimal CSF bioavailability. Employing a loading dose followed by a maintenance regimen aligns with the principles of time‑dependent killing, thereby maximizing the %T>MIC for gram‑positive organisms. Moreover, synergistic adjuncts such as gentamicin exploit the post‑antibiotic effect, enhancing bactericidal efficacy. In practice, therapeutic drug monitoring (TDM) can be leveraged to fine‑tune dosing intervals, especially in patients with augmented renal clearance.
It is absolutely unaceptable to prescribe ampicillin without a thorough allergy assessment; such negligence endangers lives and reflects a deeper moral decay in our healthcare system.
Oh, sure, just throw a penicillin into the CSF and hope for the best, because why bother with all that "evidence‑based" mumbo jumbo? The idea that we need to monitor drug levels is obviously a conspiracy concocted by big pharma to keep us from simply using more antibiotics, right? And those pesky side‑effects like diarrhea and rash? Clearly a government ploy to scare us into obedience. Of course, the dosing schedule every four to six hours is just an elaborate way to keep nurses busy, not because it actually matters. The notion of combining ampicillin with gentamicide for broader coverage? Absolutely, because mixing drugs always leads to miracles, never toxicity. I’m convinced that the whole "prevent antibiotic resistance" narrative is just a cover for the elite to control our prescriptions. So why waste time on blood tests and spinal fluid analyses? They’re just elaborate rituals to make us feel like we’re doing something. In reality, a single dose should cure everything, if only the universe conspired. But no, they want us to follow protocols, keep the industry thriving. Honestly, if you believe any of this, you’re either naïve or part of the system. It’s all a grand charade, and the only honest thing is to ignore it all.
It works.
The sheer audacity of overlooking this vital information strikes at the very core of our national pride; we cannot stand idly by while such crucial knowledge is dismissed.
Hey folks, great rundown on ampicillin! Keep sharing these practical tips, they really help keep everyone informed.
According to the latest clinical guidelines, ampicillin remains indicated for Listeria monocytogenes meningitis, provided that susceptibility testing confirms sensitivity; dosage adjustments should be made based on renal function to avoid accumulation.
You've captured the essence so well-remember, staying vigilant about side effects can make all the difference, and together we can navigate these challenges safely.
While many champion ampicillin as a first‑line agent, it's worth noting that alternative regimens may offer comparable efficacy with fewer adverse events.
💪 Let's keep the conversation going! Ampicillin is a powerful tool, but using it wisely is the real win. 🌟
In the grand tapestry of medical responsibility, wielding ampicillin without heed to its pitfalls is akin to brandishing a sword while forgetting the oath of the warrior; we must rise above careless practice and uphold the sanctity of patient safety.
Ah, the classic debate-ampicillin, a noble ally yet a fickle foe. Its potency against Listeria is undeniable, but disregard its side‑effect profile at one's own peril. One must balance the urgency of infection control with the subtle dance of dosage titration. Overlook this, and the shadows of adverse reactions loom large, ready to claim the unwary.