Pancreatic Duct Blockage: What You Need to Know
Blocked pancreatic ducts can cause sharp belly pain, digestion trouble, and serious complications if left alone. If you or someone you care for has recurring upper abdominal pain, greasy stools, or unexplained weight loss, a blocked pancreatic duct could be the reason. This page explains practical steps: how the problem shows up, how doctors check for it, and what treatments look like.
Causes & Symptoms
The most common causes are gallstones that move into ducts, chronic alcohol-related pancreatitis that scars ducts, tumors pressing on the duct (including pancreatic cancer), and strictures after injury or prior surgery. Less common causes include very high triglycerides or genetic conditions that affect the pancreas.
Symptoms vary. Expect sudden severe pain in the upper belly that may radiate to the back, nausea, vomiting, fever (if infection is present), and jaundice if bile flow is also blocked. Over time you might notice greasy, foul-smelling stools (steatorrhea) and weight loss—signs the pancreas isn’t releasing enzymes to digest food properly.
Diagnosis and Treatment
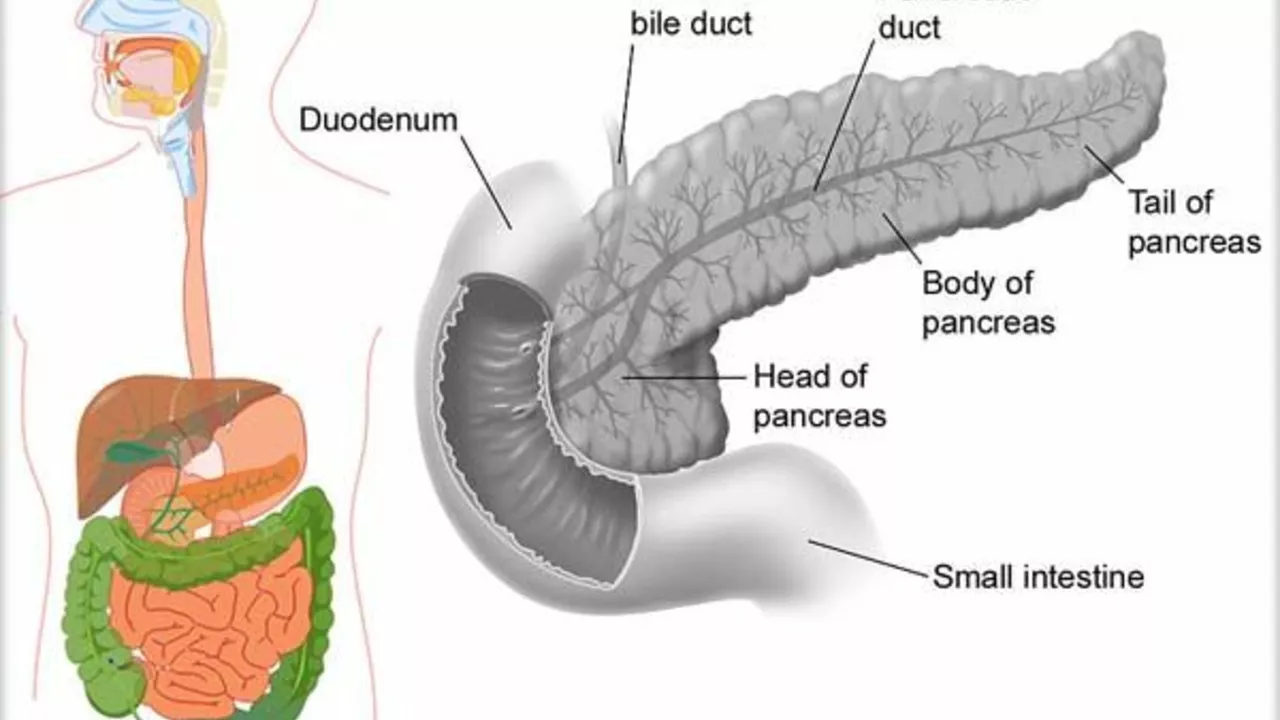
Start with blood tests for amylase, lipase, and liver tests. Imaging comes next: abdominal ultrasound, CT scan, or MRI/MRCP to see the duct and nearby structures. MRCP is noninvasive and good at spotting blockages; ERCP is both a test and a treatment tool—doctors use a camera and small instruments through the mouth to reach and open the blocked duct.
Treatment depends on the cause. If a gallstone is stuck, ERCP can remove it. For strictures or narrowing, endoscopic stents often relieve the blockage and let the duct drain. Tumors may need surgery, chemotherapy, or radiation depending on type and stage. In acute infected cases (cholangitis or infected pancreatic duct), hospitals give IV antibiotics and urgent drainage.
Other measures help too: pain control, IV fluids, and bowel rest during acute attacks. Long-term, enzyme pills can replace digestive enzymes if malabsorption happens. Your team may recommend lifestyle changes—quit alcohol, control triglycerides, and follow a low-fat diet while it heals.
What should you ask your doctor? Ask what likely caused the blockage, which test they recommend first, whether ERCP is needed now, and what are the risks and recovery time for any procedure. Also ask about enzyme replacement, diet changes, and follow-up imaging.
When to get help fast: severe, unrelenting belly pain, high fever, yellowing skin or eyes, rapid heart rate, or fainting. Those can mean infection or worsening blockage and need emergency care.
Simple prevention steps: treat gallstones if recommended, avoid heavy alcohol use, manage triglycerides with diet and meds, and keep routine check-ups if you have chronic pancreatitis. Early action often means simpler fixes and fewer complications.
Managing Pancreatic Duct Blockage: Tips for Caregivers
As a caregiver for someone dealing with pancreatic duct blockage, I've discovered a few key steps to manage this condition effectively. Firstly, it's essential to understand the dietary modifications needed, like a low-fat diet, to avoid putting extra strain on the pancreas. Monitoring for symptoms such as jaundice, weight loss, or abdominal pain is crucial for early intervention. Regular consultations with healthcare professionals and following prescribed medication regimen is also key to managing this condition. Lastly, emotional support plays a significant role in improving the patient's quality of life during this challenging time.
Keep Reading