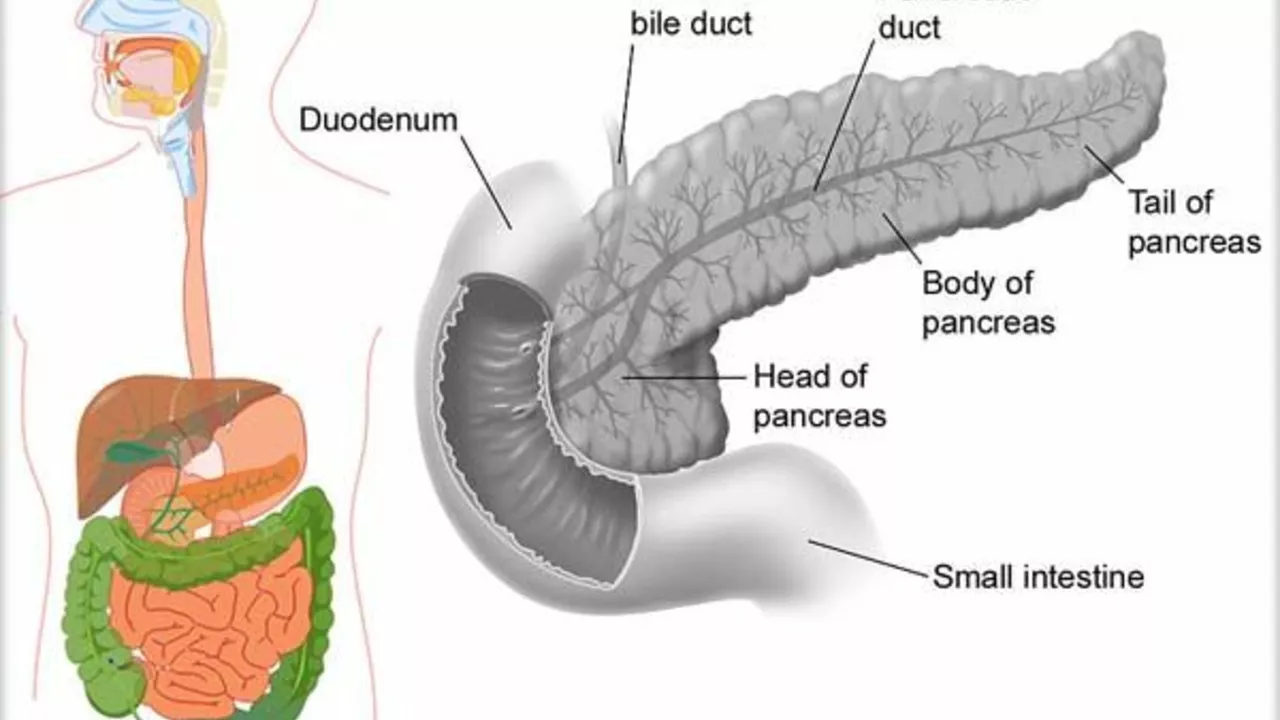
Understanding the Pancreatic Duct Blockage
As a caregiver, it's crucial to understand what pancreatic duct blockage is before diving into how to manage it. The pancreatic duct is a tube that runs from the pancreas and connects to the common bile duct just before entering the duodenum, the first section of the small intestine. Blockage of this duct often results in pancreatitis, a painful and potentially serious condition. The blockage can be caused by gallstones, tumors, or chronic pancreatitis. Understanding the cause is the first step towards effective management.
Recognizing the Symptoms
Spotting the symptoms early can lead to a quicker diagnosis and treatment. Common symptoms of pancreatic duct blockage include severe abdominal pain, jaundice (a yellowing of the skin and eyes), nausea, vomiting, and weight loss. The pain can sometimes be relieved by leaning forward or curling into a ball. As a caregiver, if you notice any of these symptoms, it's essential to seek medical attention immediately. While these symptoms can be indicative of other conditions, it's better to be safe than sorry.
Medical Treatment Options
Once a diagnosis has been made, a doctor will recommend the best course of treatment. This could include medication to relieve pain and inflammation, lifestyle changes, or in some cases, surgery. The type of treatment will largely depend on the cause of the blockage. For example, if gallstones are the culprit, the doctor may recommend surgery to remove the gallbladder. If the blockage is due to a tumor, chemotherapy or radiation therapy may be necessary. As a caregiver, it's important to understand the treatment plan and ensure that the person you're caring for is following it.
Caring for a Loved One at Home
Once the immediate crisis has passed and your loved one is back at home, your role as a caregiver will be pivotal. This will involve ensuring they take their medication on time, helping them to make necessary lifestyle changes, and monitoring them for any changes in their condition. If your loved one has been prescribed pain medication, it's important to watch for any signs of dependency. Additionally, you may need to help them adjust to a new diet, as certain foods can exacerbate the condition. This can be a challenging time, but your support can make a significant difference in their recovery.
Maintaining Your Own Wellbeing
Finally, while you're focusing on caring for your loved one, don't forget to take care of yourself. Caregiving can be emotionally and physically draining, and it's important to ensure you're looking after your own health and wellbeing. This can mean taking time out for yourself, seeking support from others in a similar situation, or even seeking professional help if you're feeling overwhelmed. Remember, you can't pour from an empty cup, so make sure to replenish yours.





5 Comments
People love to call pancreatic duct blockage a "simple" issue, but the truth is that the human body rarely gives us anything that neat. You can’t just label it and move on, because the cascade of enzymes, hormones, and emotional stress creates a tangled web. Think of the pancreas as a tiny alchemist; when its conduit gets clogged, the whole laboratory goes haywire. Caregivers often feel like they're trying to fix a leaky faucet with a sledgehammer, and that frustration is justified. So, instead of glossing over the complexity, dig deeper, question the standard recommendations, and remember that every case writes its own story.
I get that the article tries to be helpful but it could use a bit more clarity especially when describing the diet adjustments. Caregivers need clear steps not vague suggestions and the tone should stay respectful to those who are already overwhelmed the point is to help not add confusion
If you’re not American, you wouldn’t care about this.
Wow, that’s a bold claim 😒 but honestly, caring for someone with a blocked duct isn’t about patriotism, it’s about empathy. I’ve seen people act like a drama queen when the pain flare‑ups happen and then they forget to check the meds schedule 😩. It’s exhausting watching the same cycle repeat and the article kinda skims over the emotional fatigue caregivers feel. Still, credit where it’s due – the reminder to look after yourself is solid, even if it’s a bit cliché.
The physiological cascade precipitated by pancreatic duct obstruction is far more intricate than most lay explanations suggest. When the ductal lumen narrows, pancreatic secretions accumulate, precipitating autodigestion and triggering a robust inflammatory response that can swiftly evolve into necrotizing pancreatitis. This protean process is modulated not only by the mechanical impediment but also by systemic factors such as cytokine release, oxidative stress, and the patient's baseline nutritional reserves. Consequently, a caregiver’s role extends beyond mere medication administration; it encompasses vigilant monitoring of fluid balance, electrolytic homeostasis, and early recognition of subtle hemodynamic shifts. Nutritional stewardship, for instance, must balance low‑fat, high‑protein regimens while avoiding precipitous glucose excursions that could exacerbate inflammatory pathways. Moreover, the psychosocial dimension cannot be overstated – chronic stress hormones like cortisol may impair immune competence, thereby prolonging convalescence. It is incumbent upon caregivers to liaise closely with multidisciplinary teams, ensuring that radiologic surveillance, such as endoscopic retrograde cholangiopancreatography, is judiciously timed to alleviate obstruction without incurring iatrogenic trauma. In parallel, prophylactic measures against infection, including judicious use of broad‑spectrum antibiotics, should be calibrated to the patient's microbiome status. Finally, self‑care for the caregiver is not a peripheral concern but a central pillar of sustained patient support; burnout can diminish vigilance, leading to medication errors or missed clinical cues. In sum, the management of pancreatic duct blockage demands an orchestrated, evidence‑based strategy that integrates pathophysiological insight with compassionate, systematic caregiving.