Understanding mesalamine: What It Does and Who Needs It
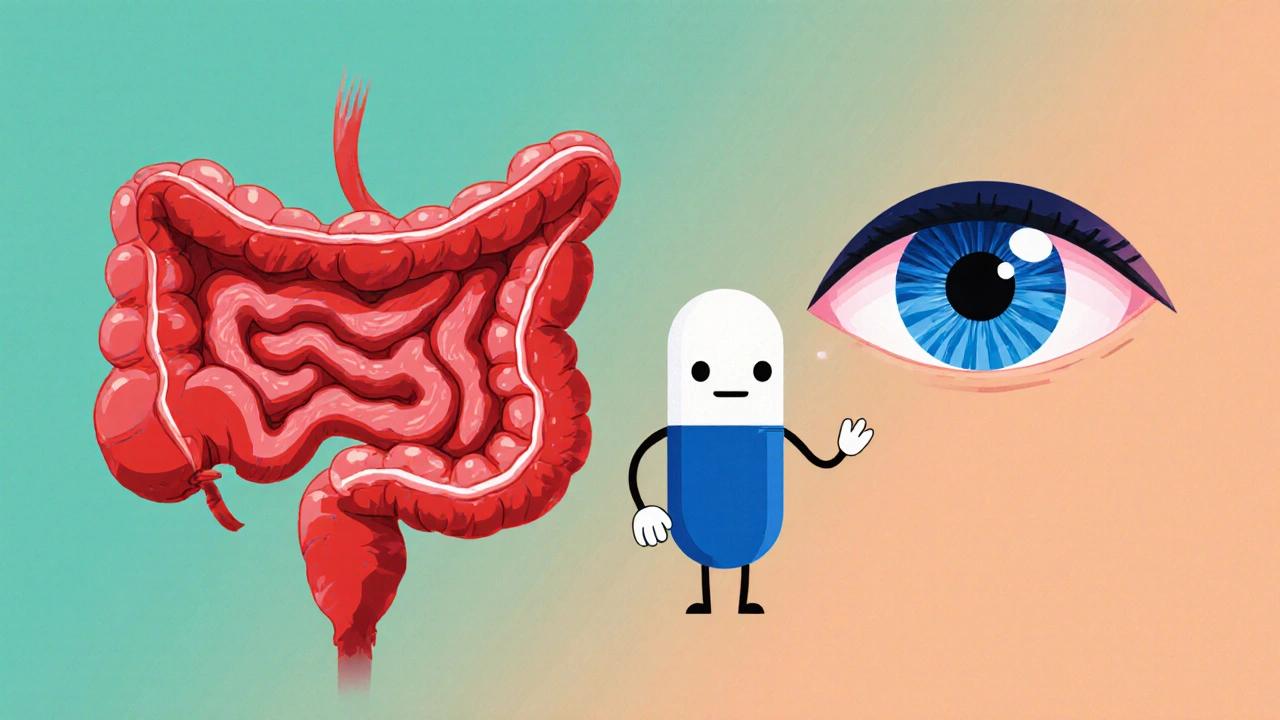
When working with Mesalamine, an oral and rectal anti‑inflammatory medication that releases 5‑aminosalicylic acid directly in the colon. Also known as 5‑ASA, it targets the lining of the large intestine to calm flare‑ups caused by ulcerative colitis. The drug is available in tablets, capsules, and suppositories, each designed to dissolve at a specific point in the gut for maximum effect. Because it works locally rather than systemically, mesalamine typically avoids the broader side‑effects seen with steroids, making it a first‑line choice for long‑term maintenance therapy.
Patients often hear the term Ulcerative colitis, a chronic inflammation of the colon that leads to bloody diarrhea, abdominal cramps, and urgency when discussing mesalamine. This condition sits under the umbrella of Inflammatory bowel disease, a group of disorders, including Crohn’s disease and ulcerative colitis, characterized by persistent gastrointestinal inflammation. The link is clear: mesalamine belongs to the 5‑ASA class, and its primary job is to reduce the inflammatory cascade that drives ulcerative colitis symptoms. Diagnosis often involves colonoscopy, blood tests, and stool studies, all of which help doctors gauge disease severity and choose the right mesalamine formulation.
How mesalamine Fits into IBD Treatment
Beyond mesalamine itself, clinicians frequently consider related drugs like sulfasalazine, a prodrug that the gut bacteria convert into both sulfapyridine and mesalamine. Sulfasalazine can be useful when patients need a combined anti‑inflammatory and antibacterial effect, but its sulfapyridine component often brings more side‑effects, such as headaches or nausea. Because of this, many doctors start patients on plain mesalamine to avoid unnecessary complications. Dosing varies with disease extent: mild left‑sided colitis may respond to a low‑dose tablet, while extensive colitis often requires higher doses spread across multiple daily administrations. Topical forms—suppositories or enemas—are added when inflammation is confined to the rectum, delivering the drug right where it’s needed.
Monitoring treatment response is a key part of any mesalamine regimen. Regular blood work checks for rare but serious liver or kidney issues, while stool calprotectin levels can signal hidden inflammation. Endoscopic surveillance every 1‑3 years helps catch dysplasia early, especially in long‑standing disease. Lifestyle tweaks—like a low‑residue diet during flare‑ups, staying hydrated, and stress management—enhance drug effectiveness. Patients who maintain a consistent dosing schedule and attend routine check‑ups usually experience fewer hospitalizations and a better quality of life.
Below you’ll find a curated collection of articles that dive deeper into drug comparisons, symptom management, and practical tips for living with IBD. Whether you’re weighing mesalamine against other 5‑ASA options, looking for cost‑saving strategies, or seeking advice on dietary adjustments, these posts give you actionable insight to make informed decisions about your treatment plan.
How Mesalamine Helps Manage Eye Complications in IBD Patients
Discover how mesalamine, a common IBD drug, can also help manage eye inflammation like uveitis and episcleritis, with tips, evidence, and patient advice.
Keep Reading