MEN1 – Understanding Multiple Endocrine Neoplasia Type 1
When working with MEN1, a hereditary syndrome that triggers tumors in several endocrine glands. Also known as Multiple Endocrine Neoplasia Type 1, it shapes how doctors monitor calcium, hormone levels, and tumor growth across the body.
One of the most common manifestations is a pituitary adenoma, a usually benign tumor in the pituitary gland. This growth can alter prolactin or growth hormone output, leading to headaches, vision changes, or menstrual irregularities. Knowing the link between MEN1 and pituitary adenomas helps patients and clinicians catch symptoms early and decide on medication or surgery.
Another hallmark is parathyroid hyperplasia, which causes excess parathyroid hormone and high calcium levels. Symptoms range from kidney stones to bone pain, and the condition often shows up before any pancreatic or pituitary issues. Regular blood tests for calcium and vitamin D become essential parts of an MEN1 management plan.
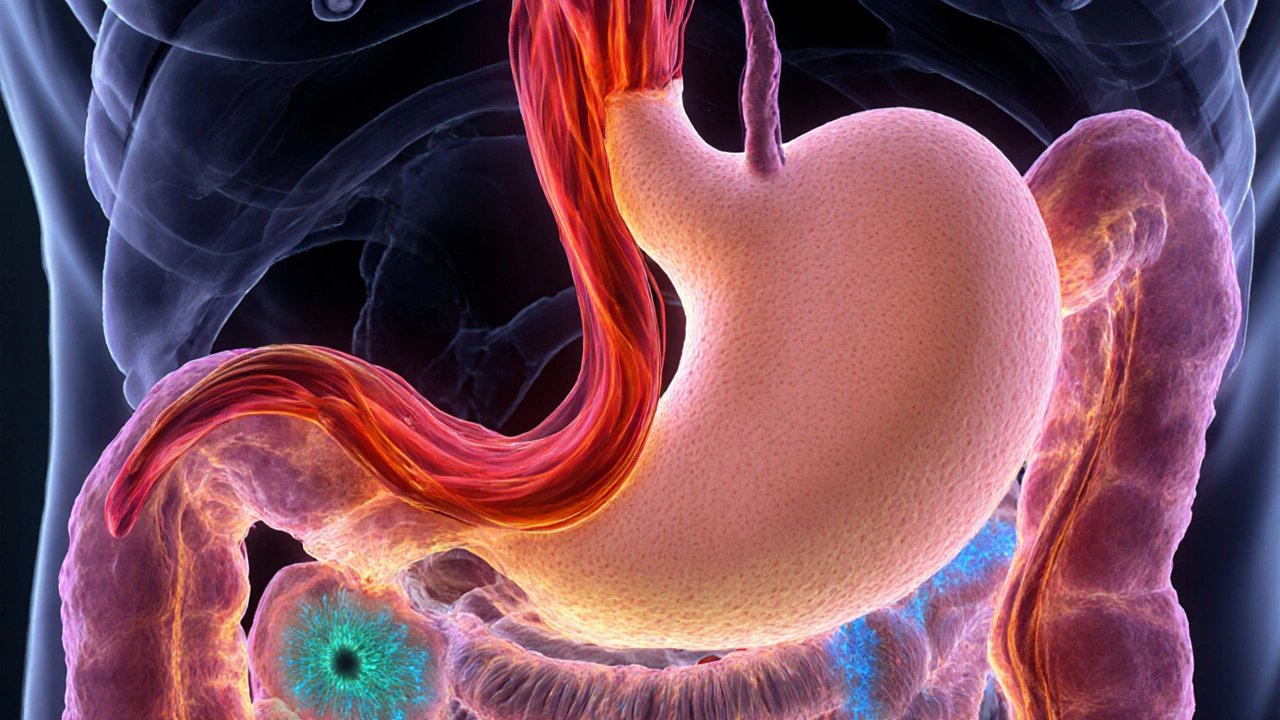
Many people associate MEN1 with pancreatic neuroendocrine tumors. These can secrete insulin, gastrin, or other hormones, leading to low blood sugar, ulcers, or skin changes. Early imaging and hormone assays can spot these tumors while they’re still small, which dramatically improves treatment outcomes.
Because MEN1 runs in families, genetic testing is a game‑changer. Identifying the MEN1 gene mutation lets relatives know their risk, guides surveillance schedules, and can even influence family planning decisions. The test itself is a simple blood draw, but interpreting results requires a genetics counselor or an endocrinologist familiar with the syndrome.
Why MEN1 matters for treatment choices
The syndrome creates a web of interrelated health issues. For instance, treating a parathyroid problem may affect calcium balance, which in turn influences bone health and kidney function. Likewise, medication that suppresses a pituitary adenoma could interact with drugs used for pancreatic tumors. Understanding these connections—MEN1 encompasses pituitary adenoma, requires genetic testing, and influences hormone therapy—helps clinicians build a coordinated care plan.
Patients often wonder how lifestyle fits into the picture. Simple steps like staying hydrated, limiting processed foods high in sodium, and getting regular check‑ups can keep calcium swings in check. When a pancreatic tumor is active, dietary adjustments such as smaller, frequent meals can stabilize blood sugar spikes. These practical tips complement the medical strategies discussed in the articles below.
Screening schedules are another key piece. Most guidelines suggest starting calcium and hormone panels in the early teens for anyone with a confirmed MEN1 mutation, followed by imaging every few years. This proactive approach catches tumors before they cause major symptoms, which is why early detection through genetic testing is so valuable.
Our collection of posts dives deep into each of these topics. You’ll find side‑by‑side drug comparisons for HCG, guidance on managing obesity‑related uric acid, and practical advice on heartburn prevention—all relevant because MEN1 often intertwines with metabolic and hormonal disorders. The articles also cover medication safety, dosage tips, and how to choose the right therapy for each organ system involved.
Ready to explore the specifics? Below you’ll discover detailed guides on drug options, condition management, and actionable steps that can help you or a loved one navigate life with MEN1. Let’s get into the resources that can make a real difference.
Zollinger-Ellison Syndrome Pathophysiology Explained
Explore how gastrin‑producing tumors drive extreme acid secretion in Zollinger‑Ellison syndrome, its genetic links, symptoms, diagnosis, and treatment.
Keep Reading