Interstitial Lung Disease: Causes, Symptoms, and What You Need to Know
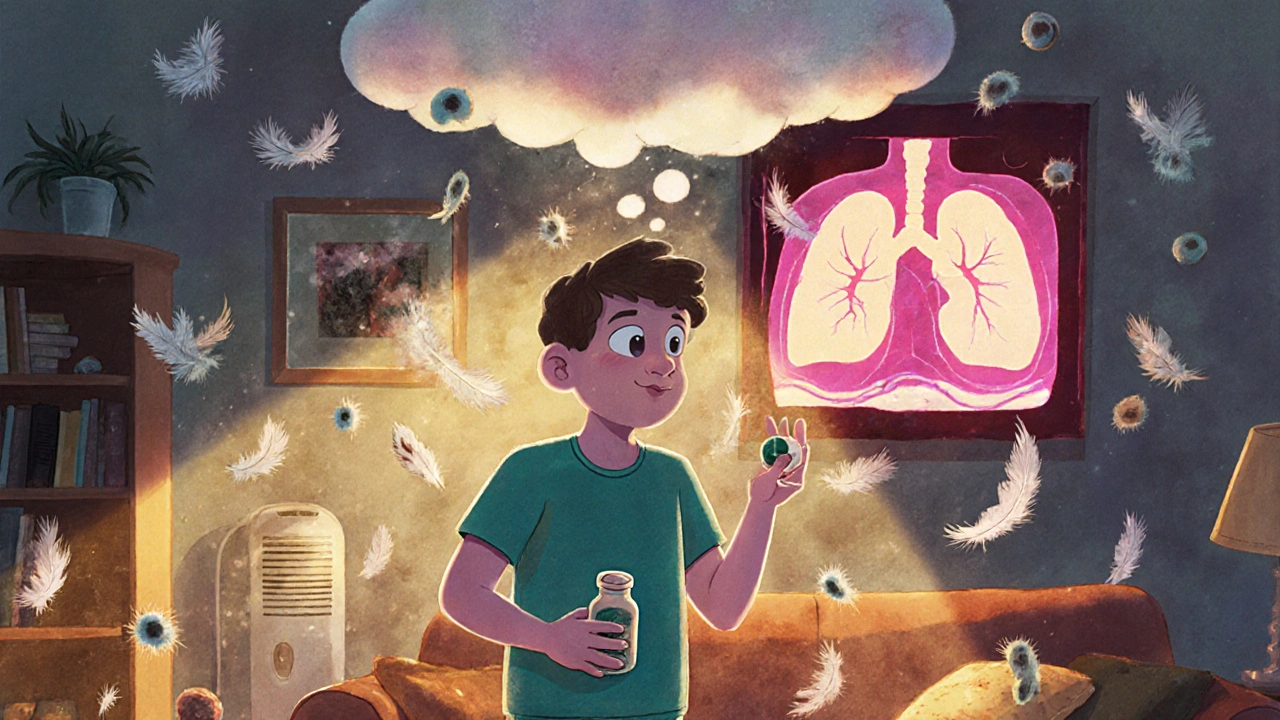
When your lungs get stiff and scarred from inflammation, it’s often interstitial lung disease, a group of over 200 disorders that damage the tissue around the air sacs in the lungs. Also known as pulmonary fibrosis, it makes it harder for oxygen to get into your bloodstream, leaving you breathless even during simple tasks like walking to the mailbox. Unlike asthma or COPD, which affect the airways, interstitial lung disease attacks the space between the air sacs — the interstitium — where oxygen swaps into your blood. This damage is often slow, sneaky, and irreversible, but catching it early can still make a big difference.
Many people don’t realize they have it until they’re winded climbing stairs or feel a dry cough that won’t go away. Some cases are linked to autoimmune diseases like rheumatoid arthritis or scleroderma. Others come from long-term exposure to dust, asbestos, or certain medications. Even some antibiotics and heart drugs can trigger it. There’s no single test to confirm it — doctors usually need a mix of CT scans, lung function tests, and sometimes a biopsy to see the scarring. The good news? New treatments are slowing progression better than ever, and oxygen therapy, pulmonary rehab, and lifestyle changes can help you stay active longer.
It’s not just about the lungs. People with this condition often deal with fatigue, joint pain, and even heart strain because the heart has to work harder to push blood through stiff lungs. That’s why managing other health issues — like high blood pressure or diabetes — becomes even more important. If you’ve been told your oxygen levels are low or your chest X-ray looks "hazy," don’t ignore it. The posts below cover real stories and practical advice: how to tell if your cough is just a cold or something worse, what meds help reduce scarring, how to avoid triggers like mold or bird droppings, and why some people need lung transplants while others stabilize for years with the right care.
What you’ll find here isn’t theory — it’s what people actually deal with. From understanding test results to navigating insurance for oxygen equipment, these articles cut through the noise. You’ll learn how to talk to your pulmonologist, spot warning signs before a flare-up, and avoid common mistakes like skipping rehab or mislabeling side effects as allergies. This isn’t a one-size-fits-all condition, and the right info can change how you live with it — not just survive it.
Hypersensitivity Pneumonitis from Medications: Cough and Breathlessness
Hypersensitivity pneumonitis is caused by breathing in environmental triggers like mold or bird droppings - not medications. But some drugs can cause similar cough and breathlessness symptoms. Learn how to tell the difference and what to do next.
Keep Reading