When you start coughing and can’t catch your breath, it’s natural to worry. Maybe it’s a cold. Maybe it’s allergies. But what if it’s something deeper - something tied to a medicine you’ve been taking? Many people assume that if a drug causes lung symptoms like cough and breathlessness, it must be hypersensitivity pneumonitis. But that’s not quite right. Hypersensitivity pneumonitis (HP) isn’t caused by pills, injections, or IV meds. It’s caused by breathing in tiny particles from the environment - mold, bird droppings, dust from hay, or even humidifier gunk. Medications don’t trigger HP the way these airborne antigens do.
What Hypersensitivity Pneumonitis Actually Is
Hypersensitivity pneumonitis is an immune reaction in the lungs. It happens when you repeatedly inhale something your body sees as foreign. Your immune system overreacts, sending inflammatory cells into the tiny air sacs (alveoli) of your lungs. That’s what causes the cough, the tight chest, and the feeling that you can’t get enough air - even when you’re just walking to the kitchen.
This isn’t asthma. Asthma narrows your airways. HP attacks the lung tissue itself. It’s not contagious. It’s not cancer. But left unchecked, it can scar your lungs for life. The damage shows up on a high-resolution CT scan as ground-glass opacities, mosaic patterns, and in later stages, honeycombing - signs of irreversible fibrosis.
There are three forms:
- Acute: Symptoms hit 4 to 8 hours after heavy exposure - fever, chills, cough, breathlessness. You feel awful. But if you get away from the trigger, you often recover in 1-2 days.
- Subacute: You’re exposed a little bit, every day or every week. Symptoms creep up over weeks: fatigue, dry cough, worsening breathlessness during activity. You might think you’re just getting out of shape.
- Chronic: Years of low-level exposure. You lose weight. Your fingers club. Your lungs stiffen. This is the dangerous stage. About 30-50% of chronic cases develop permanent scarring, even with treatment.
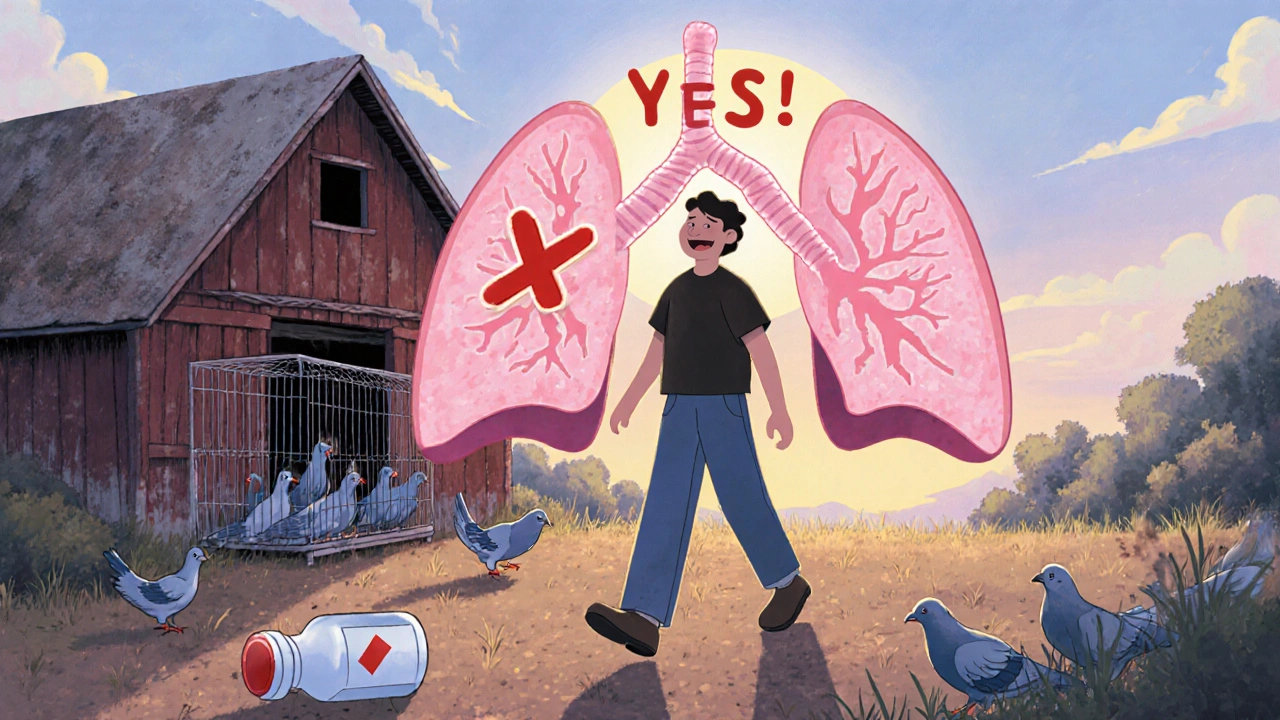
Common triggers? Bird fancier’s lung (from pigeon or parrot droppings), farmer’s lung (from moldy hay), mushroom picker’s lung, and humidifier lung (from contaminated water systems). None of these involve swallowing a pill.
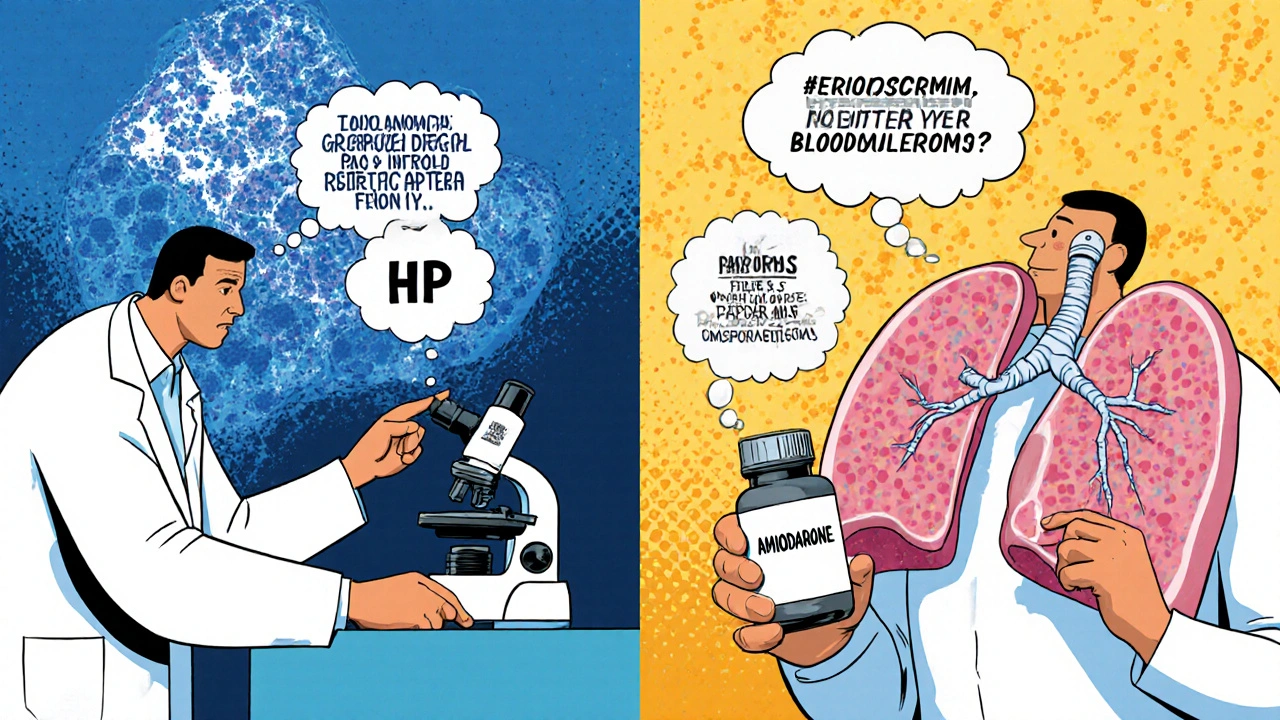
Why Medications Don’t Cause True Hypersensitivity Pneumonitis
There’s a big difference between drug-induced lung injury and hypersensitivity pneumonitis. Medications like amiodarone, nitrofurantoin, or bleomycin can damage the lungs. They cause cough, breathlessness, and even fibrosis. But they don’t cause HP.
Why? Because HP requires inhalation of a specific antigen - something your lungs directly breathe in - that triggers a very particular immune response: poorly formed granulomas, lymphocyte-rich inflammation around the small airways, and a pattern called bronchiolocentric inflammation. These features show up in lung biopsies of HP patients.
Drug-induced lung injury? It looks different. Amiodarone causes phospholipid buildup. Nitrofurantoin triggers acute interstitial pneumonitis. Bleomycin causes direct cell death. These reactions don’t form granulomas the same way. They don’t show the same lymphocyte pattern. They’re not triggered by inhalation. They’re systemic.
Major medical sources - the Merck Manual, the American Lung Association, the Pulmonary Fibrosis Foundation - all list environmental causes. None list medications as a cause of hypersensitivity pneumonitis. The term ‘medication-induced hypersensitivity pneumonitis’ is a misnomer. It’s not a recognized diagnosis in pulmonology guidelines.
What Medications Actually Do to the Lungs
If you’re on a drug and suddenly develop a dry cough and shortness of breath, it’s not HP - but it could still be serious. Here are the most common offenders:
- Amiodarone: Used for irregular heart rhythms. Can cause a chronic, fibrotic lung injury that mimics HP. Often mistaken for it. Up to 5% of long-term users develop lung damage.
- Nitrofurantoin: An antibiotic for UTIs. Can cause acute lung injury within days - fever, cough, low oxygen. Usually reversible if caught early.
- Bleomycin: A chemotherapy drug. Causes oxidative damage to lung cells. Can lead to fatal pulmonary fibrosis, especially in older patients or those with kidney problems.
- Checkpoint inhibitors: Used in cancer immunotherapy (like pembrolizumab). Can trigger immune-related pneumonitis - a different mechanism, but still lung inflammation.
- NSAIDs and sulfonamides: Rarely, these can cause eosinophilic pneumonia, which looks like a drug reaction but has different cell types in the lung fluid.
The key difference? With these drugs, symptoms don’t improve when you leave a room or avoid a dusty attic. They don’t come and go with exposure. They’re tied to the drug’s presence in your bloodstream.
How to Tell the Difference
Doctors use four things to figure out if it’s HP or drug injury:
- History: Did you start the cough after moving into a new house with a moldy basement? Or after starting amiodarone last month?
- Imaging: HP shows mosaic attenuation and air trapping on expiratory CT scans. Drug injury often looks more like patchy ground-glass or organizing pneumonia.
- Blood and lung fluid tests: HP patients often have high lymphocytes in bronchoalveolar lavage fluid (>40%). Drug reactions may show eosinophils or no clear pattern.
- Biopsy: The gold standard. HP has granulomas clustered around small airways. Drug injury has different patterns - like diffuse alveolar damage or fibrosis without granulomas.
One of the biggest clues? If your symptoms get worse when you’re at home - but vanish on vacation - it’s likely HP. If your symptoms got worse after you started a new pill - and don’t change with location - it’s likely a drug reaction.
What to Do If You Suspect Lung Damage
Don’t wait. Cough and breathlessness from lung injury can worsen fast. Here’s what to do:
- Stop the drug immediately - but only under your doctor’s supervision. Never quit a heart or cancer drug on your own.
- See a pulmonologist - not just your primary care doctor. They’ll order the right scans and tests.
- Get a CT scan - high-resolution CT is essential. A regular chest X-ray won’t show early changes.
- Ask about bronchoscopy - a small tube into the lungs can collect fluid to check for lymphocytes or eosinophils.
- Track your symptoms - write down when they happen, what you were doing, and what meds you took.
If it’s a drug reaction, stopping the medication often leads to full recovery - especially if caught early. Corticosteroids like prednisone may be used for a few weeks to calm the inflammation.
If it’s HP, the treatment is simpler - and harder: avoid the trigger. No more bird feeders. No more humidifiers. No more dusty barns. If you can’t avoid it, you’ll need steroids - and even then, you might still develop fibrosis.
Long-Term Outlook
HP from environmental causes has a better chance of recovery if caught early. About 70-80% of acute cases bounce back completely. But if you keep breathing in the trigger, your lungs scar. Chronic HP has a 5-year survival rate of only 50-80%, depending on how much scarring you already have.
Drug-induced injury? If you catch it early and stop the drug, most people recover fully. Amiodarone damage can linger for years - even after stopping. Bleomycin injury can be deadly. But unlike HP, you don’t need to change your whole life - just your meds.
The bottom line? Medications can hurt your lungs. But they don’t cause hypersensitivity pneumonitis. They cause something else - drug-induced interstitial lung disease. And that’s just as important to recognize.
What You Can Do Today
If you’re on a medication and have a new cough or shortness of breath:
- Don’t ignore it. Don’t assume it’s just aging or being out of shape.
- Check the drug’s side effects. Look up your exact medication online - not just the brand name, but the generic too.
- Write down your exposure history: Do you have birds? Do you clean humidifiers? Do you work in agriculture or a lab?
- Ask your doctor: ‘Could this be a drug reaction? Could it be hypersensitivity pneumonitis?’
- If you’re told it’s HP - ask: ‘What am I breathing in? Can you prove it?’
Many people spend months chasing asthma or COPD, when the real culprit is a pill they’ve been taking for years. The right diagnosis saves your lungs - and your life.
Can medications cause hypersensitivity pneumonitis?
No. True hypersensitivity pneumonitis is caused by inhaling environmental antigens like mold, bird proteins, or dust from hay. Medications can cause lung injury, but they trigger different types of inflammation - not the granulomas and lymphocyte patterns that define HP. The term ‘medication-induced HP’ is misleading and not recognized in medical guidelines.
What are the most common drugs that cause lung damage?
The top culprits include amiodarone (for heart rhythm), nitrofurantoin (for UTIs), bleomycin (a chemotherapy drug), and immune checkpoint inhibitors like pembrolizumab. These can cause cough, breathlessness, and lung scarring, but they don’t cause hypersensitivity pneumonitis. They cause drug-induced interstitial lung disease.
How do I know if my cough is from a drug or from the environment?
If your symptoms improve when you’re away from home - like on vacation - and return when you come back, it’s likely an environmental trigger (like mold or birds). If your symptoms started after beginning a new medication and don’t change with location, it’s likely drug-related. A pulmonologist can confirm this with imaging, lung fluid tests, and sometimes a biopsy.
Is hypersensitivity pneumonitis reversible?
In the acute phase - if you stop exposure right away - yes, recovery is often complete. In subacute or chronic cases, especially with scarring, the damage may be permanent. Early diagnosis and strict avoidance of the trigger are the only ways to prevent long-term harm.
Should I get a lung biopsy if I have cough and breathlessness?
Not always. Doctors usually start with a detailed history, CT scan, and bronchoalveolar lavage. A biopsy is only needed if the diagnosis is unclear - for example, if it’s hard to tell if it’s HP, a drug reaction, or another lung disease. Biopsies are invasive, so they’re reserved for cases where the treatment plan depends on the exact diagnosis.





9 Comments
Thank you for this incredibly clear breakdown. I’ve seen so many patients confuse drug-induced lung injury with hypersensitivity pneumonitis, and the consequences can be devastating when the wrong intervention is pursued. The distinction between environmental antigen exposure and systemic drug toxicity isn’t just academic-it changes everything about management, prognosis, and quality of life. This post should be required reading for every primary care provider.
Let me tell you, I’ve been in pulmonology for 27 years, and I still see this mistake happen every single month. Someone comes in with a cough, they’ve been on amiodarone for six months, and the first thing the ER doc says is, ‘Could this be bird fancier’s lung?’ No. No, it’s not. It’s amiodarone toxicity. You don’t need to ask if they have a parrot-you need to ask if they’ve been taking their heart meds. And if you miss it, you’re looking at irreversible fibrosis. This isn’t just semantics. It’s survival.
It is an unfortunate and pervasive epistemological error in contemporary clinical discourse to conflate disparate pathophysiological mechanisms under the umbrella of a single diagnostic label. Hypersensitivity pneumonitis, by definition, necessitates an inhaled particulate antigen that elicits a T-cell-mediated granulomatous response localized to the bronchioloalveolar units. Medications, by virtue of their systemic pharmacokinetics and distinct molecular interactions, induce parenchymal injury through cytotoxic, oxidative, or immune-mediated pathways that lack the characteristic bronchiolocentric lymphocytic infiltration and non-caseating granulomas. The misuse of terminology not only misinforms patients but also corrupts the precision required for evidence-based therapeutic decision-making. One must not allow linguistic laziness to compromise clinical acuity.
OMG YES. I had a patient last week who was convinced her humidifier was the problem-turned out it was her new blood pressure med. She cried when we told her she didn’t have to give up her plants or her humidifier 😭 Just stop the drug and boom-she was breathing again in 3 weeks. So glad someone’s finally saying this out loud!! 🙌
Of course medications don’t cause ‘hypersensitivity pneumonitis.’ That’s what they told us about asbestos too. And then the lawsuits started. Funny how the pharmaceutical industry prefers to call it ‘drug-induced interstitial lung disease’-so clean, so clinical, so not their fault. But if you’re coughing up blood and your CT looks like Swiss cheese, does it really matter what label they put on it? The pill still poisoned your lungs. The system still failed you. The only difference? They won’t have to pay for your transplant.
As someone who has worked in both academic pulmonology and global health settings, I can confirm that this distinction is critically under-taught in low-resource environments. In rural India, for instance, a patient with nitrofurantoin-induced pneumonitis is often misdiagnosed as having tuberculosis due to overlapping symptoms and lack of imaging access. The terminology barrier compounds the diagnostic delay. This post provides not just a clinical correction, but a global public health imperative: precise language saves lives, especially where diagnostics are scarce.
It makes me wonder-why do we keep trying to fit complex biological reactions into neat little boxes? We’ve got this urge to name everything, to categorize, to make it feel controllable. But lungs are messy. Immune responses are messy. Maybe ‘hypersensitivity pneumonitis’ and ‘drug-induced injury’ are just two different doors leading to the same room: inflammation that kills. Maybe the real question isn’t what to call it, but how to listen better-to the patient’s story, to their environment, to the timeline of their symptoms. The label matters, yes. But the listening matters more.
They say it’s not HP. But have you seen the FDA’s adverse event reports? There are over 12,000 cases of ‘drug-induced HP’ since 2010. Coincidence? Or is this a cover-up? The same companies that made Vioxx are now quietly rebranding lung damage as ‘interstitial disease’ so they don’t have to recall drugs. They don’t want you to know that your antidepressant or diabetes pill is slowly turning your lungs to stone. Check the PACER database. Look at the whistleblower filings. This isn’t science-it’s corporate spin.
And let’s not forget: when you misdiagnose drug injury as HP, you tell the patient to stop using their humidifier… while they keep taking amiodarone. That’s not just wrong-it’s dangerous. I had a man who moved three times, bought air purifiers, quit his job to avoid ‘mold exposure’-all while his lungs were being destroyed by a pill he’d been told was ‘safe.’ He finally got diagnosed only after his oxygen saturation dropped below 85%. Don’t let your patients chase ghosts while the real poison sits in their medicine cabinet.