One glass of grapefruit juice can be harmless for most people. But if you're taking an immunosuppressant after a transplant, that same glass could land you in the hospital. This isn't a myth. It's not a warning on a label you can ignore. It's a real, life-threatening interaction backed by decades of research - and it’s still catching people off guard.
Why Grapefruit Is Dangerous With Immunosuppressants
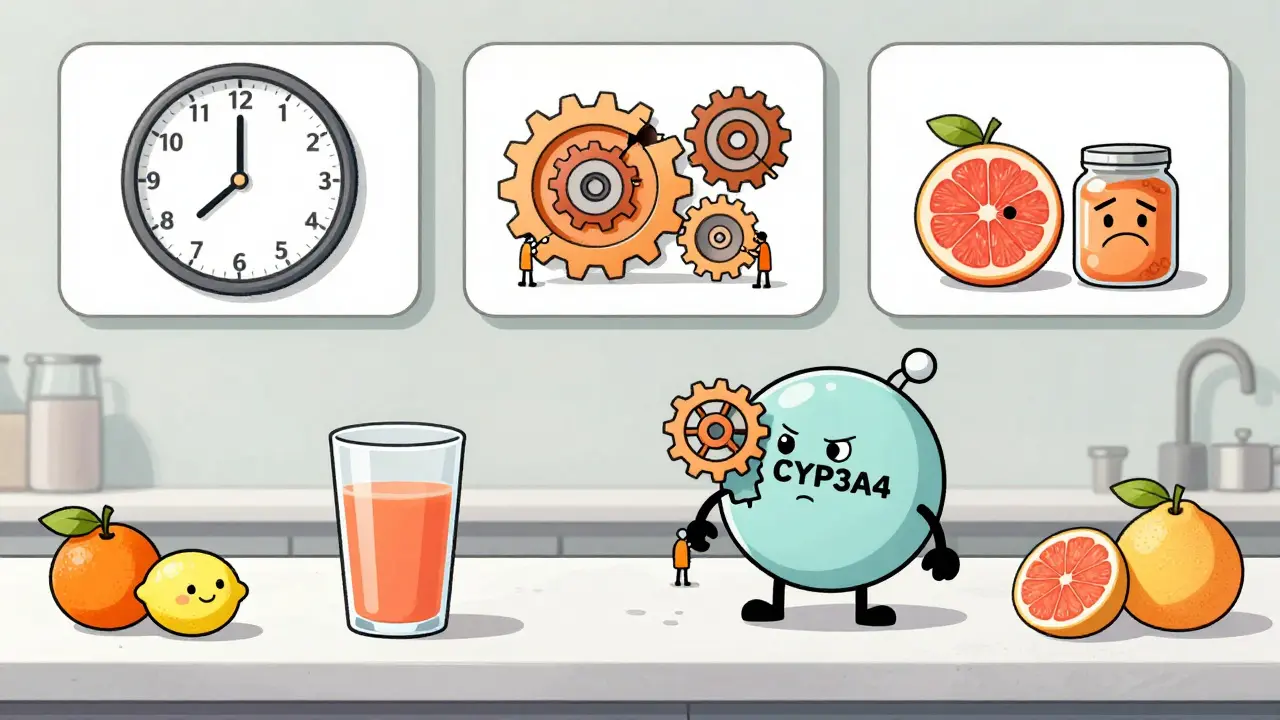
Grapefruit doesn’t just make your morning smoothie tastier. It contains chemicals called furanocoumarins, mainly 6',7'-dihydroxybergamottin and bergamottin. These compounds don’t just disappear after you swallow them. They lock onto an enzyme in your gut called CYP3A4 - the same enzyme that’s supposed to break down your immunosuppressant drugs before they enter your bloodstream. When CYP3A4 is blocked, your body can’t process the drug the way it should. Instead of 20-50% of the dose getting into your blood (the normal range for these medications), you might get 150%, 200%, or even 300% more. That’s not a small increase. It’s a spike that pushes your drug levels into the toxic zone. The three main immunosuppressants affected are:- Cyclosporine (Sandimmune, Neoral)
- Tacrolimus (Prograf, Envarsus XR, Astagraf XL)
- Sirolimus (Rapamune)
- Cyclosporine’s safe range: 100-400 ng/mL
- Tacrolimus’s safe range: 5-15 ng/mL
- Sirolimus’s safe range: 4-12 ng/mL
How Long Does the Effect Last?
Most people think if they eat grapefruit at breakfast and take their pill at night, they’re safe. That’s a dangerous assumption. The inhibition of CYP3A4 isn’t temporary. It’s irreversible. Once the enzyme is blocked, your body has to make new ones to replace them. That takes time - up to 72 hours. A 2005 study in Clinical Pharmacology & Therapeutics showed that even 72 hours after drinking 8 ounces of grapefruit juice, CYP3A4 activity was still reduced by 24%. That means if you have grapefruit on Monday, your body is still vulnerable on Thursday. If you take your immunosuppressant on Thursday, you’re still at risk. This isn’t about timing your meals. It’s about complete avoidance.What Counts as Grapefruit?
It’s not just the fruit you eat. It’s not just the juice you drink. It’s everything.- Whole grapefruit
- Grapefruit juice (even freshly squeezed)
- Grapefruit extract in supplements
- Grapefruit-flavored sodas or candies
- Pomelo (a close relative)
- Seville oranges (used in marmalade)
Real Consequences: Stories From Patients
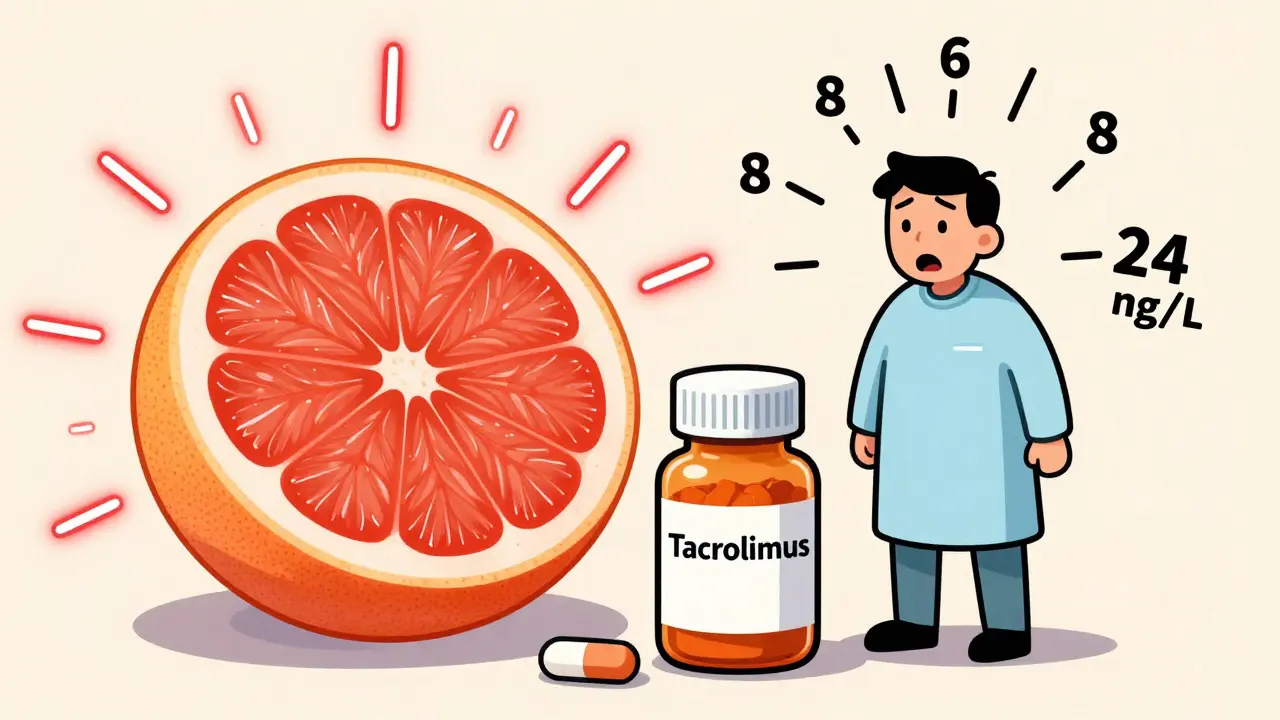
Behind the numbers are real people. One kidney transplant recipient posted on the American Transplant Foundation forum about being hospitalized with acute kidney injury after eating half a grapefruit. His tacrolimus level jumped from 8.2 ng/mL to 24.7 ng/mL in 36 hours. His doctor said he was lucky he didn’t lose the transplant. Another user on Reddit described shaking, nausea, and high potassium levels after drinking grapefruit juice once - “my doctor said this is why they tell us NEVER to have it.” Transplant pharmacists at Mayo Clinic reviewed 2021-2022 cases and found that 15-20% of unexpected immunosuppressant toxicity cases were linked to undisclosed grapefruit use. People didn’t think it was a big deal. They didn’t realize it was dangerous. They didn’t know the warning applied to them.What Doctors and Regulators Say
The FDA has been clear since 2010: grapefruit interactions must be labeled on medications. Cyclosporine’s official label now says in bold: “CONCOMITANT USE WITH GRAPEFRUIT IS CONTRAINDICATED.” The American Academy of Family Physicians (AAFP) issued a guideline in 2006 - still in effect - that says patients should stop eating grapefruit for at least 72 hours before starting any drug that interacts with it. That’s not a suggestion. That’s a medical standard. Dr. David Huang, a pharmacologist with the FDA, says: “High levels of immunosuppressants can have many negative effects, including a higher risk of infections, kidney problems, and high blood pressure.” And Dr. David Bailey, the researcher who discovered this interaction in 1989, found that grapefruit juice increased felodipine levels by 260%. The same mechanism applies to immunosuppressants.What You Should Do
If you’re on any immunosuppressant:- Avoid all grapefruit products - no exceptions. Not even once. Not even a bite.
- Check your medication guide. Look for the list of foods and drinks to avoid. If it’s not clear, ask your pharmacist.
- Ask about alternatives. If you love citrus, stick to oranges, tangerines, or lemons. They’re safe.
- Tell your transplant team. If you accidentally eat grapefruit, call them immediately. Don’t wait for symptoms.
- Monitor your levels. If exposure happens, your doctor should check your drug levels within 3-5 days and may reduce your dose by 25-50% until levels stabilize.

Why This Keeps Happening
You’d think after 34 years of warnings, everyone would know. But here’s the problem:- Many patients don’t remember the warning. They were told once, years ago, and forgot.
- Some think “natural” means safe. Grapefruit is healthy - full of vitamin C, fiber, potassium. That makes it harder to believe it’s dangerous.
- Older adults - who make up 40% of transplant recipients - often eat grapefruit for heart health. They’re not trying to break rules. They’re trying to stay healthy.
- Even pharmacists sometimes miss it. A 2023 British Liver Trust survey found 68% of transplant patients were unaware of the severity of the risk.
What’s New in 2025
The risk isn’t going away. It’s growing. In 2023, the American Society of Health-System Pharmacists added everolimus (Zortress) to the list of high-risk drugs. More transplant patients are now on this drug - and they’re at risk too. Johns Hopkins launched a mobile app in January 2023 that scans your medication barcode and instantly flags grapefruit interactions. It’s not perfect, but it’s a step forward. Research is also looking at activated charcoal as a possible way to reduce the interaction - but it’s still experimental. Don’t rely on it. The bottom line: there’s no safe workaround. No “just a little.” No “I’ll have it on weekends.”Final Reminder
You took a pill to keep your new organ alive. Grapefruit doesn’t just interfere with that pill - it can undo everything. This isn’t a suggestion. It’s a rule. And breaking it has consequences you can’t afford to learn the hard way.When your life depends on a drug, what you eat matters more than you think.






14 Comments
I dont know why people are so shocked by this. Grapefruit is just another fruit that some idiot thought was healthy. My cousin got hospitalized after eating one post-kidney transplant. He thought it was "natural" so it was fine. Lol. No its not. Your body is a machine. Dont feed it garbage.
Canada says no grapefruit. Why? Because we dont play around with life.
Stop pretending nature is always safe.
Also why is everyone using emojis like its a dating app? Grow up.
Thank you for this incredibly detailed and vital post. As a transplant recipient myself, I cannot emphasize enough how crucial this information is. I have been strictly avoiding all citrus varieties except for sweet oranges for over seven years now. Even the smallest amount of grapefruit can lead to catastrophic consequences.
It is heartbreaking to see how many individuals are unaware of this interaction, especially those who associate "natural" with "safe." We must continue to educate our communities with compassion and clarity.
Thank you for including the FDA and AAFP guidelines-this lends authority and urgency to the message. 🙏
Let’s be real. This isn’t about grapefruit. It’s about the medical-industrial complex exploiting fear to control behavior. Why don’t they just make a safer drug? Why do we need to live in constant fear of a fruit?
Also, if the enzyme is permanently inhibited, why are we still prescribing these drugs? Sounds like bad pharmacology to me.
And don’t get me started on the FDA. They approved this crap in the first place. Now they’re acting like they’re the hero. Wake up. This is corporate negligence dressed up as public health.
I’m so grateful for this post. My dad had a liver transplant last year and I had no idea about grapefruit until he told me. We’ve been reading labels like our lives depend on it (which they do).
He used to love grapefruit for breakfast. Now he eats oranges and smiles like he won the lottery.
Also-Seville oranges in marmalade?? I had no idea. Going to throw out the whole jar tonight. 🍊❤️
You know what’s more dangerous than grapefruit? The fact that people still don’t read medication guides. I’ve seen patients take statins with grapefruit and then blame the doctor when they get rhabdomyolysis.
It’s not the fruit’s fault. It’s the patient’s refusal to take responsibility. The FDA label says "CONTRAINDICATED." That’s not a suggestion. That’s a legal warning.
And yet, we still have people saying, "I only had a little."
Little kills. Always has.
There’s something poetic about this. We’re told to eat more fruit, more natural foods, more "superfoods"-but the body doesn’t care about marketing. It cares about biochemistry.
Grapefruit is like a silent saboteur. Beautiful on the outside. Deadly inside.
It reminds me of how we romanticize nature while ignoring its complexity.
I think we need to stop treating our bodies like gardens and start treating them like laboratories.
And yes, I cried when I read about the guy whose tacrolimus spiked. That’s not a statistic. That’s a person.
I’m not saying this to be mean, but if you’re dumb enough to eat grapefruit after being told not to, you don’t deserve a transplant.
People think medicine is magic. It’s not. It’s math. It’s chemistry. It’s discipline.
You get one chance. One. And you blow it because you wanted a taste of citrus?
It’s not just selfish. It’s a betrayal of the donor.
And yes, I know it’s harsh. But someone has to say it.
OMG I just realized my mom buys that grapefruit juice from Trader Joe’s. She’s on cyclosporine. I’m literally running to the kitchen rn.
Also-pomelo?? Wait, so that big weird citrus I ate in Hawaii last year??
Y’all. I need a new grocery list. 🙏
Wait so does this mean I can’t have grapefruit-flavored kombucha? I’ve been drinking it every morning for my gut health. 😳
India has no grapefruit but we have pomelo and it is dangerous too. My uncle died after eating one. No warning. No label. No education. This is why people die in developing countries. Not because of the fruit. Because of the silence.
I get it. Grapefruit is bad. But what about bergamot tea? Earl Grey? That’s from the same plant. Are we supposed to give up tea too?
And what about the people who can’t afford expensive alternatives? What if oranges are out of season and grapefruit is the only citrus they can get?
This feels like a rich person’s problem dressed up as a medical rule.
Nah this is all fake. Grapefruit is fine. I’ve been eating it with my tacrolimus for 3 years. My levels are perfect.
Doctors just want you scared so you’ll take more pills.
Also I read on a blog that grapefruit helps detox your liver. So it’s probably helping.
I didn’t know Seville oranges were dangerous. I love marmalade. I just threw out my entire jar.
Also-my mom used to say grapefruit was good for your skin. I guess she was wrong.
Anyway, I’m gonna start reading the little pamphlets now. I promise. 🙈
Let me tell you something. I’ve been studying this for 12 years. I’ve read every study. I’ve talked to the researchers. I’ve met the families.
This isn’t just about grapefruit. This is about how our healthcare system fails people. We give them a pill. We give them a warning. We never teach them why.
People don’t understand enzymes. They don’t understand pharmacokinetics. They don’t know what a narrow therapeutic index means.
So they eat the grapefruit.
And then they die.
And we call it an accident.
It’s not an accident. It’s a systemic failure.
And until we start teaching patients like they’re human beings-not just compliance targets-we’re going to keep losing people to things like this.
So yeah. Grapefruit is dangerous.
But the real villain? The silence.