Drug-Induced Pneumonitis: Causes, Risks, and What to Watch For
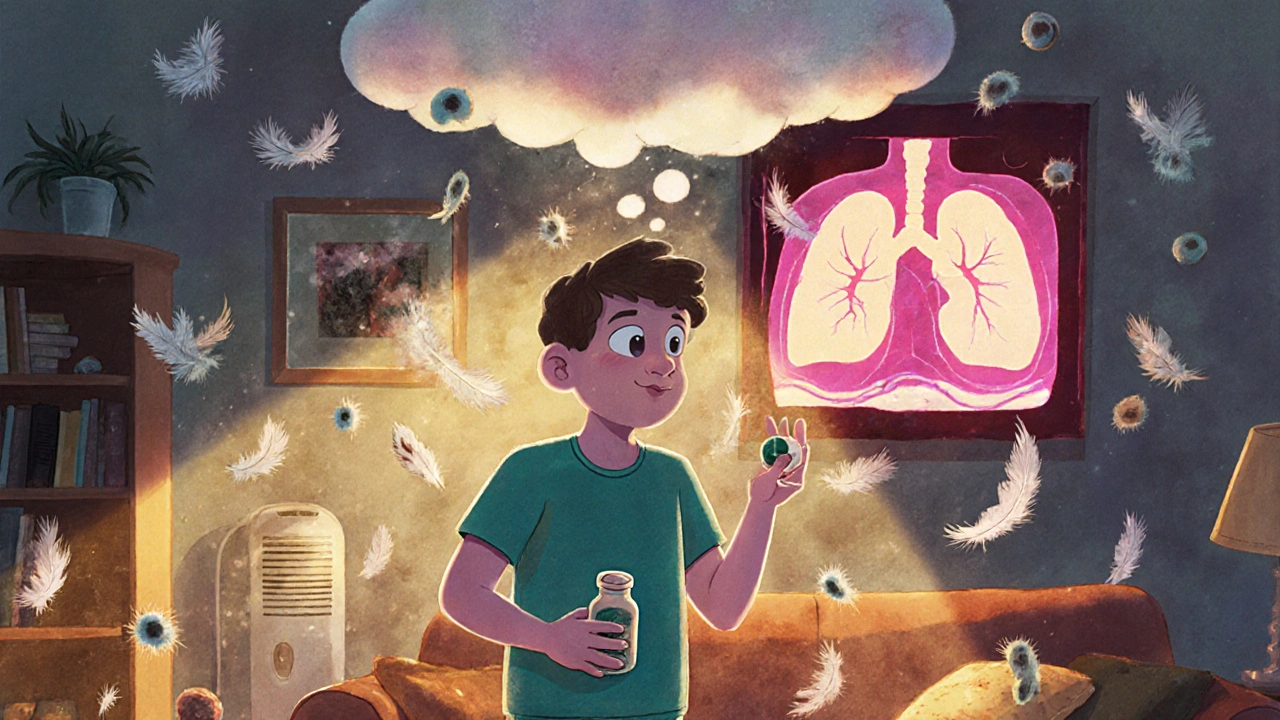
When your lungs react badly to a medicine you’re taking, it’s not always just a cough or mild shortness of breath. Drug-induced pneumonitis, a type of lung inflammation triggered by medications. Also known as medication-induced lung injury, it’s a hidden risk that many people don’t realize is tied to their prescriptions. This isn’t an allergy—it’s a toxic reaction. Think of it like your immune system misreading a drug as an invader and attacking your lung tissue instead. It can happen with antibiotics, heart meds, chemotherapy drugs, even some supplements. And it often looks like pneumonia, asthma, or just getting older—so it’s missed a lot.
Some of the most common culprits include amiodarone, a heart rhythm drug known to cause lung scarring over time, nitrofurantoin, a urinary tract antibiotic that can damage lungs after weeks or months, and methotrexate, used for autoimmune diseases and sometimes cancer, which can cause sudden lung inflammation. Even drugs like checkpoints inhibitors, used in cancer immunotherapy, are linked to this. You might not feel sick right away. Symptoms can creep in over days or weeks: dry cough, trouble breathing during light activity, fatigue, or low-grade fever. If you’ve started a new drug and your lungs feel off, don’t assume it’s just a cold. It could be your lungs reacting to something you swallowed.
What makes this tricky is that most doctors don’t test for it unless they’re already suspicious. Blood tests won’t show it. A regular chest X-ray might look normal. The real clue? A high-res CT scan showing patchy inflammation, plus a history of recent drug exposure. Stopping the drug early often reverses it. Waiting too long can lead to permanent scarring. That’s why knowing which meds carry this risk matters. You’re not overreacting if you ask your pharmacist or doctor: "Could this be affecting my lungs?" The posts below cover real cases, how to spot early signs, what drugs to watch out for, and how to talk to your care team without sounding paranoid. You’ll find advice on distinguishing this from infections, how to track symptoms over time, and what to do if your symptoms don’t go away after stopping a drug. This isn’t theoretical—it’s something that happens to real people, often because no one connected the dots between the pill and the breathlessness.
Hypersensitivity Pneumonitis from Medications: Cough and Breathlessness
Hypersensitivity pneumonitis is caused by breathing in environmental triggers like mold or bird droppings - not medications. But some drugs can cause similar cough and breathlessness symptoms. Learn how to tell the difference and what to do next.
Keep Reading