Diabetic Peripheral Neuropathy: What to Know and Do
Up to half of people with diabetes will develop some nerve damage in their feet or hands. That sounds scary, but knowing the signs and the right steps can prevent ulcers, infection, and long-term loss of feeling.
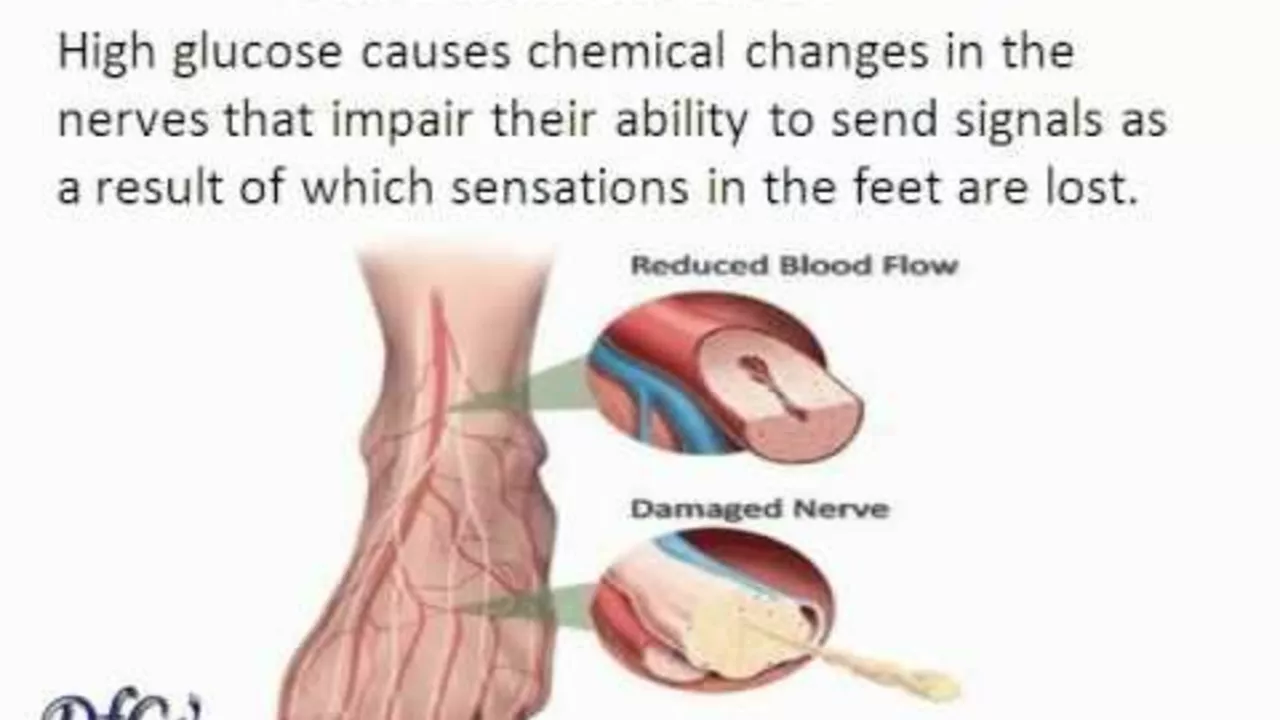
Diabetic peripheral neuropathy happens when high blood sugar injures small nerve fibers. The longer your diabetes goes uncontrolled, the higher the risk. Other factors that raise risk include smoking, high blood pressure, high cholesterol, and long diabetes duration.
Symptoms & Diagnosis
Symptoms often start slowly. You might notice:
- Numbness, tingling, or burning in your toes or feet.
- Pain that feels sharp, electric, or like pins and needles.
- Loss of balance or foot weakness.
- Increased sensitivity to touch or, paradoxically, less ability to feel heat and cold.
If you have symptoms, your clinician will do a focused exam. A simple monofilament test checks protective feeling in the foot. Vibration testing and reflex checks are common. For unclear cases, nerve conduction studies and electromyography show how well nerves send signals.
Treatment and Daily Care
Control blood sugar first. Tight glucose control lowers the chance of neuropathy getting worse. Aim for targets you and your clinician set together; sudden tight control isn’t right for everyone, so personalize the plan.
Pain treatments include medicines that work on nerve pain, not classic opioids. First-line options are gabapentin, pregabalin, and duloxetine. Topical options like lidocaine patches or capsaicin cream help some people with localized pain. If medicines cause side effects or don’t help, your doctor may try other options, including TENS therapy or referral to a pain specialist.
Foot care is non-negotiable. Check your feet every day for cuts, blisters, redness, or swelling. Use a mirror or ask someone to help if you can’t see the bottoms. Wear well-fitting shoes and clean socks. Never walk barefoot. Trim nails straight across and seek podiatry care for thick nails or ingrown toenails. If you find a sore that won’t heal within a few days, get medical attention right away—early treatment prevents infection and amputation.
Other practical steps: stop smoking, lower blood pressure and cholesterol, and stay active. Regular moderate exercise improves circulation and can reduce pain. If you take metformin, ask your clinician to check vitamin B12 levels—low B12 can worsen neuropathy.
When to call your doctor now: sudden weakness in a foot or leg, a hot swollen foot, or a new ulcer. These need urgent attention. Also call if pain keeps you from sleeping or working despite treatment.
Consider simple balance and foot-strengthening exercises—heel raises, toe curls, and short daily walks. These lower fall risk and help circulation. Review all medicines with your clinician; some drugs worsen neuropathy. Join a diabetes education program for ongoing support and ask about referral to neurology or podiatry if symptoms progress. Get help early.
The Importance of Early Detection and Treatment for Diabetic Peripheral Neuropathy
In my latest research, I've been exploring the crucial importance of early detection and treatment for Diabetic Peripheral Neuropathy (DPN). This condition, affecting nerves predominantly in the feet and legs, often goes undiagnosed until it's too late and irreversible damage is done. By identifying symptoms early, such as tingling or numbness, we can slow its progression and manage pain effectively. Early treatment also decreases the risk of serious complications. Thus, regular check-ups are key to leading a healthier, safer life with diabetes.
Keep Reading