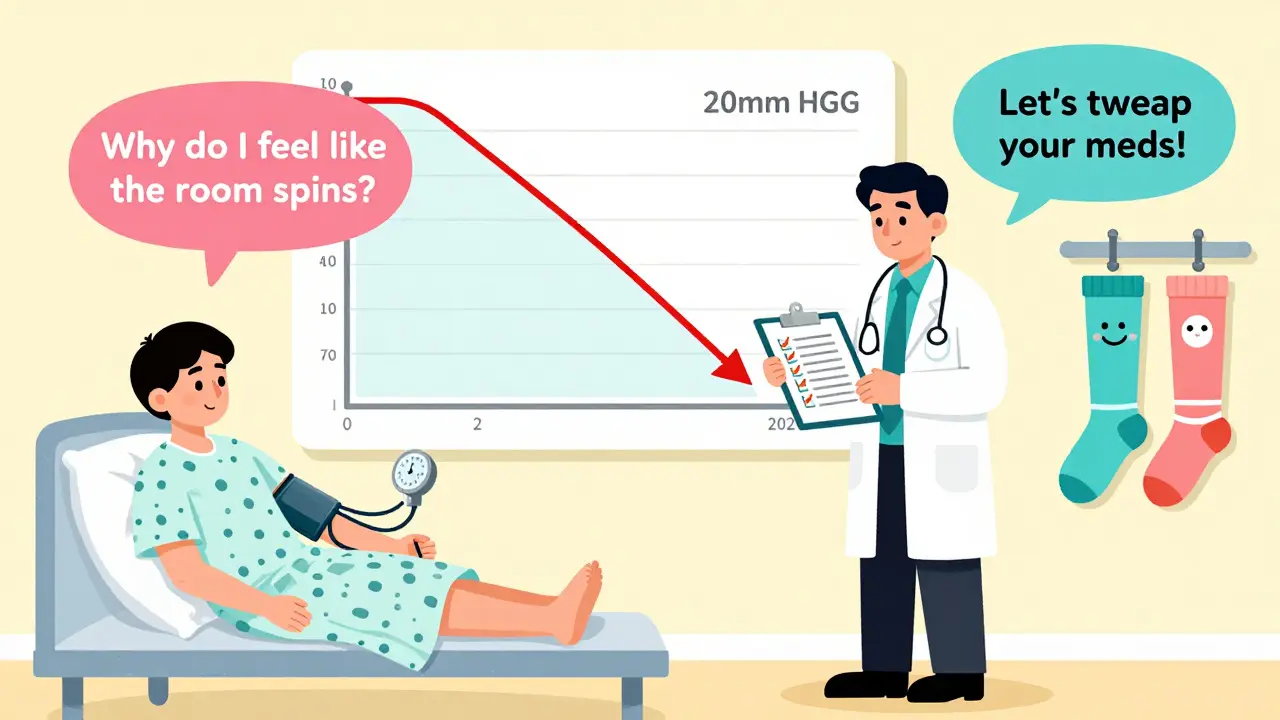
Standing up too fast and feeling like the room is spinning? That dizzy spell isn’t just bad luck-it could be your medications. Orthostatic hypotension, or orthostatic hypotension, is when your blood pressure drops suddenly as you rise from sitting or lying down. This causes dizziness, blurred vision, or even fainting. It’s not rare. In fact, up to 30% of older adults on multiple medications experience it. And here’s the thing: most of these cases are directly tied to drugs you’re already taking.
What Exactly Happens When You Stand Up?
Your body has a built-in system to keep blood flowing to your brain when you move. When you stand, gravity pulls blood down toward your legs. Normally, your nerves and blood vessels react in under a second-tightening arteries, increasing heart rate, and pushing blood upward. But when medications interfere with this system, your blood pressure plummets instead. The medical standard for diagnosing orthostatic hypotension is a drop of 20 mm Hg in systolic pressure or 10 mm Hg in diastolic pressure within three minutes of standing. And if you feel lightheaded at the same time? That’s not coincidence-it’s confirmation.Which Medications Are Most Likely to Cause This?
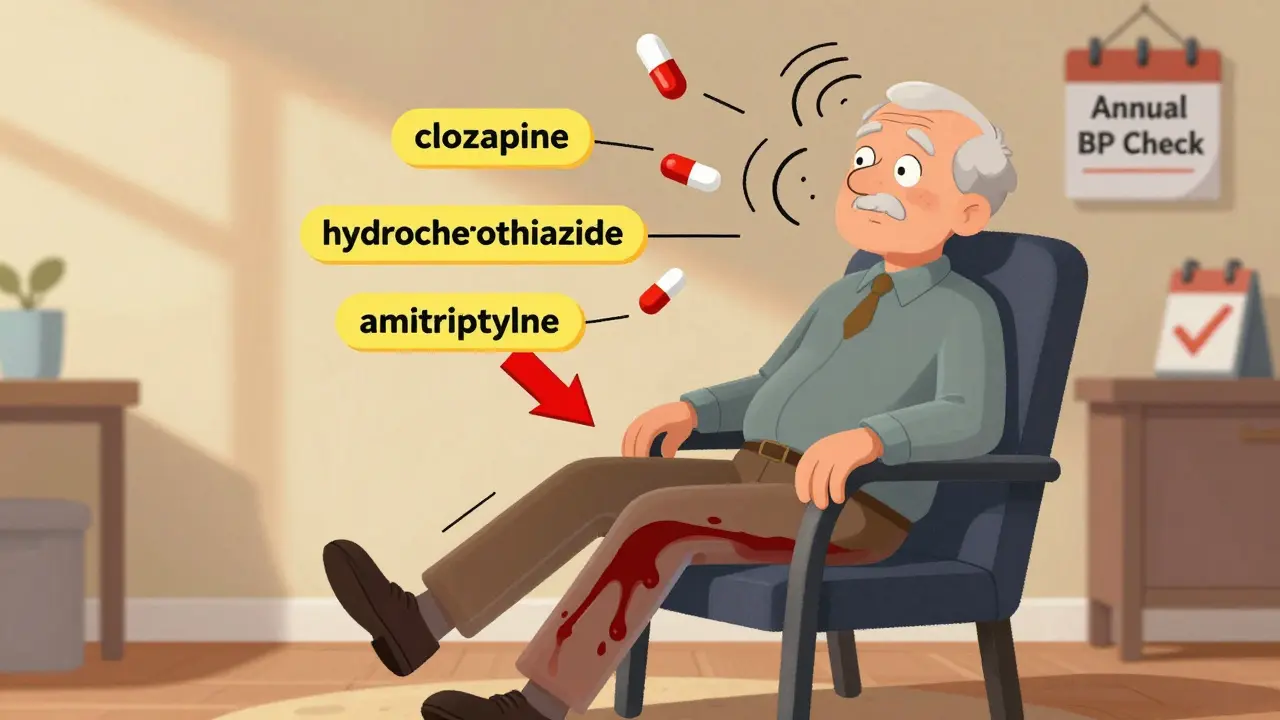
Not all drugs cause this problem equally. Some are far more dangerous than others. Here are the top offenders, backed by clinical data:- Antipsychotics like clozapine, quetiapine, and chlorpromazine: These affect brain chemicals that control blood pressure. Up to 40% of people taking high doses report dizziness on standing. One Reddit user described fainting twice after starting quetiapine-his blood pressure dropped from 128/82 to 92/61 in just two minutes.
- Alpha-blockers (used for prostate issues and high blood pressure): Medications like doxazosin and terazosin relax blood vessels too much. They carry a 2.8 times higher risk of orthostatic hypotension compared to other blood pressure drugs.
- Diuretics (water pills): Hydrochlorothiazide and furosemide reduce blood volume. If you’re dehydrated or sweating a lot, your body can’t compensate. A patient in Cleveland Clinic’s forum saw his falls stop completely after stopping hydrochlorothiazide-within 72 hours.
- Tricyclic antidepressants: Amitriptyline and nortriptyline block nerve signals that regulate blood pressure. They increase OH risk by over 3 times.
- Opioids: Morphine, oxycodone, and hydrocodone slow down the autonomic nervous system. About 15-25% of elderly patients on opioids develop symptoms. The risk jumps 2.3 times if combined with alcohol or benzodiazepines.
- Levodopa: Used for Parkinson’s, it causes orthostatic hypotension in 30-50% of users. It’s one of the most common reasons older Parkinson’s patients fall.
Here’s the kicker: it’s not just one drug. The more medications you take, the worse it gets. People on four or more drugs have 5.7 times higher risk than those on one or two. And if you’re over 70? Your risk is more than three times higher than someone under 60.
Why Is This So Dangerous?
Dizziness might feel like a nuisance, but it’s not harmless. Every fall carries risk-broken hips, head injuries, long hospital stays. People with medication-induced orthostatic hypotension have a 15-30% higher chance of falling. And the long-term effects are even scarier. Studies show a 24-32% increase in 10-year mortality risk for those with persistent OH. Why? Because low blood pressure to the brain over time may contribute to cognitive decline. It’s not just about falling-it’s about your brain slowly being starved of oxygen.And here’s what most people don’t realize: up to 40% of people with orthostatic hypotension have no symptoms. They feel fine-until they don’t. That’s why doctors should check blood pressure both lying and standing during routine visits, especially for older adults on multiple meds.
What Can You Do About It?
The good news? Medication-induced orthostatic hypotension is often reversible. About 65-80% of patients improve significantly once their meds are adjusted. Here’s what works:- Review every medication with your doctor. Don’t assume your blood pressure pill is the only culprit. Antidepressants, pain meds, and even some sleep aids can be the hidden cause.
- Stand up slowly. Don’t jump out of bed. Sit on the edge for 30 seconds. Then stand still for another 30. Let your body adjust.
- Drink more water. Aim for 2-2.5 liters a day. Dehydration makes everything worse. Add a pinch of salt to your water if your doctor approves-it helps retain fluid.
- Wear compression stockings. These squeeze your legs and help push blood back up. They’re simple, cheap, and surprisingly effective.
- Avoid alcohol and large meals. Both dilate blood vessels and drop pressure further. Eat smaller meals, and skip the wine with dinner if you’re prone to dizziness.
If these steps don’t help, your doctor may consider switching you to a safer alternative. For example, instead of clozapine, they might try ziprasidone-its OH risk is only 5-10%. Or swap hydrochlorothiazide for a different blood pressure drug that doesn’t deplete volume as much.
What Doctors Are Doing Differently Now
In 2022, the American Geriatrics Society updated its Beers Criteria-essentially a list of drugs that are risky for older adults. Twelve medications are now flagged for orthostatic hypotension. Since then, 68% of U.S. primary care clinics have started screening patients over 65. That means your doctor should now be checking your blood pressure in both positions during annual visits.There’s also new guidance from the American Heart Association in 2023. If lifestyle changes don’t work, they now recommend midodrine-a drug that tightens blood vessels-as a first-line treatment. It’s taken three times a day and reduces symptoms by about 65% in clinical trials.
And the future? Researchers are testing personalized medicine approaches. Some trials are looking at genetic markers to predict who’s most likely to develop OH from certain drugs. Imagine a blood test that tells your doctor, “Don’t give this patient levodopa-it’ll drop their BP too hard.” That’s coming soon.

Real Stories, Real Results
A 78-year-old man in Melbourne was falling once a week. He was on lisinopril, hydrochlorothiazide, amitriptyline, and oxycodone. His doctor cut the diuretic and switched the antidepressant to a safer option. Within five days, his dizziness vanished. He hasn’t fallen since. Another woman, 72, started on quetiapine for anxiety. She got dizzy every time she walked to the kitchen. Her pharmacist flagged it. She switched to a different antipsychotic. Within two weeks, she was back to gardening without fear. These aren’t rare cases. They’re textbook examples of what happens when medication risks aren’t reviewed.When to See a Doctor
If you’ve felt dizzy, blurry, or faint when standing up-especially if it’s happened more than once-don’t ignore it. Write down when it happens, how long it lasts, and what you were doing. Bring that list to your doctor. Ask: “Could any of my medications be causing this?”And if you’re caring for an older relative, watch for subtle signs: slow walking, avoiding stairs, holding onto furniture, or refusing to get up after meals. These aren’t just “getting old.” They might be signs of low blood pressure.
Final Thoughts
Orthostatic hypotension isn’t something you just have to live with. It’s a warning sign-a signal that your medication list might need a tune-up. The good news? You don’t need surgery, expensive tests, or new gadgets. Just a careful review of your pills, a few simple habits, and a doctor who listens. Millions of people feel dizzy on standing every day. Most of them don’t realize it’s fixable. You don’t have to be one of them.Can orthostatic hypotension go away on its own?
Yes, in many cases-especially if it’s caused by medication. Once the drug is stopped or switched, symptoms often improve within days to weeks. Around 70-85% of medication-induced cases resolve after proper adjustment. But if it’s caused by nerve damage (like in Parkinson’s), it’s less likely to fully disappear. That’s why identifying the cause matters.
Is orthostatic hypotension the same as low blood pressure?
No. Normal low blood pressure (hypotension) means your BP is low all the time, even when lying down. Orthostatic hypotension is a sudden drop that only happens when you stand up. Someone can have normal BP while sitting but crash when standing-that’s orthostatic hypotension. It’s about change, not just number.
Can drinking more water help with dizziness on standing?
Absolutely. Dehydration reduces blood volume, making it harder for your body to maintain pressure when standing. Drinking 2-2.5 liters of water daily can improve symptoms significantly. Adding a little salt (if your kidneys are healthy) helps your body hold onto fluid. Many patients notice less dizziness within just a few days of increasing fluid intake.
Are compression stockings really effective?
Yes, and they’re one of the most underused tools. Compression stockings squeeze your legs and help push blood back toward your heart and brain. Studies show they reduce dizziness in about 60% of patients. You don’t need medical-grade ones-over-the-counter support socks (15-20 mm Hg pressure) work well for most people. Wear them in the morning before you stand up.
Should I stop my medication if I feel dizzy?
Never stop a medication without talking to your doctor. Some drugs, like blood pressure or antidepressants, can cause dangerous rebound effects if stopped suddenly. Instead, track your symptoms, note when they happen, and bring them to your doctor. They can help you safely adjust the dose or switch to a safer alternative.
Why do some people get this and others don’t?
It’s a mix of age, meds, and biology. Older adults have weaker baroreceptor reflexes-the body’s natural blood pressure regulators. People taking four or more drugs have five times higher risk. Genetics also play a role: some people’s bodies naturally compensate less well for posture changes. But the biggest factor? Polypharmacy. The more pills you take, the higher your chance of a drug interaction that drops your BP.
Can exercise help with orthostatic hypotension?
Yes-but not all types. Strength training, especially for the legs, helps improve circulation and vascular tone. Walking regularly also trains your body to respond better to posture changes. Avoid sudden bursts of activity. Try seated exercises if standing makes you dizzy. Avoid exercising in hot rooms or right after meals, as heat and digestion can worsen symptoms.
Is orthostatic hypotension more common in winter?
Yes. Cold weather causes blood vessels to constrict, which can make your body less responsive to posture changes. Also, people drink less water in winter, and indoor heating can cause dehydration. Combine that with flu season and more medications being used, and orthostatic hypotension spikes in colder months. Stay hydrated and dress warmly when going outside.




10 Comments
This is why America's healthcare is a joke. Doctors hand out pills like candy and never check if they're killing you slowly. I saw my uncle fall three times in six months because they kept giving him that damn hydrochlorothiazide. No one cared until he broke his hip. Now he's in a nursing home. All because they'd rather prescribe than think.
And don't even get me started on the FDA. They approve these drugs faster than fast food. You want to live to 80? Stop taking half your medicine and start asking questions. Or just keep on trusting the system. Your choice.
Orthostatic hypotension is just the tip of the iceberg when it comes to polypharmacy in geriatrics. The real issue is the lack of pharmacokinetic profiling in elderly populations-most clinical trials exclude patients over 75, yet we prescribe these cocktails to them anyway. It’s not negligence, it’s institutionalized ignorance.
And let’s not pretend compression stockings are a solution. They’re a Band-Aid on a hemorrhage. We need de-prescribing protocols, not lifestyle hacks masquerading as medicine.
I never knew this was so common. My dad takes five meds and gets dizzy every time he stands up. He just says it’s ‘old age.’ Now I’m going to take him to the doctor and ask about each pill. Thank you for writing this. Maybe we can fix this before something worse happens.
Also, water and salt? That sounds too simple to work… but I’ll try it.
Medications cause OH. Fix the meds. Done.
I’ve seen this with my mom. She was on amitriptyline for years, never told anyone she felt like she was going to pass out every time she got up. I didn’t realize it was the medicine until I read this. We switched her to a different one last month. She’s been walking around the house without holding onto the walls. It’s small, but it’s huge.
Thank you for saying this out loud. So many people suffer in silence.
Oh wow, so we’re blaming the drugs now? Not the fact that people are too lazy to stand up slow? Or that they drink soda instead of water? Or that they think ‘I’m old, I’m supposed to be dizzy’?
Meanwhile, the real problem is that doctors are overworked and underpaid, so they prescribe and move on. But hey, let’s just blame the pills. Much easier than fixing the system.
Also, compression socks? Yeah, because nothing says ‘I care about your health’ like squeezing your legs like a sausage casing. Real innovation, folks.
LOL. You people actually think drinking water and standing slow fixes this? That’s cute. My grandma was on 7 meds and still fell through the floor. She died in the ER. No amount of salt or socks would’ve saved her. This isn’t a lifestyle issue-it’s a pharmaceutical massacre.
And don’t get me started on midodrine. That’s a band-aid on a bullet wound. They’re selling you hope while the system keeps writing scripts like it’s a video game. Wake up.
Also, ‘genetic markers coming soon’? Yeah right. Big Pharma will bury that until they can patent the test and charge $2000 for it.
Man, this hit different. My brother-in-law’s a paramedic-he’s seen more elderly folks collapse on their kitchen floors than most doctors. He says the same thing every time: ‘They’re not dying of old age. They’re dying of prescriptions.’
I used to think dizziness was just part of getting older. Now I see it for what it is: a silent scream from a body that’s been overworked by pills it never asked for.
And that story about the woman who went back to gardening? That’s the kind of win we need more of. Not flashy, not expensive. Just someone getting their life back because someone finally listened.
Actually, the 2022 Beers Criteria update only flagged 11 medications-not 12-for orthostatic hypotension. You’re misquoting the guideline. Also, midodrine isn’t first-line per AHA 2023-it’s second-line after non-pharmacologic interventions fail. And the 65-80% improvement rate? That’s only true for *medication-induced* cases, not all OH. You’re conflating etiologies.
And let’s not forget: levodopa-induced OH is often refractory because it’s neurodegenerative, not pharmacological. You need fludrocortisone or droxidopa in those cases, not just ‘switch the drug.’
This post is dangerously oversimplified. People will stop their meds based on this and end up in the ER.
lol i read this whole thing and i still dont know if i should drink more water or just quit my meds. my doc says ‘just stand slow’ like im a robot. but i tried that and i still passed out in the shower. now i sit on the toilet for 10 mins before i get up. its kinda sad.
also who the hell has time to wear socks all day? i got kids and a job. and my wife says i smell like old people now. thanks for nothing.