When someone is struggling with obsessive-compulsive disorder, finding the right medication can feel like searching for a key in a dark room. You know there’s one that fits - but which one? For many people, the answer lies in two main classes of drugs: SSRIs and clomipramine. These aren’t just random prescriptions. They’re the only medications proven through decades of research to reliably reduce OCD symptoms when used correctly.
Why SSRIs Are the First Choice
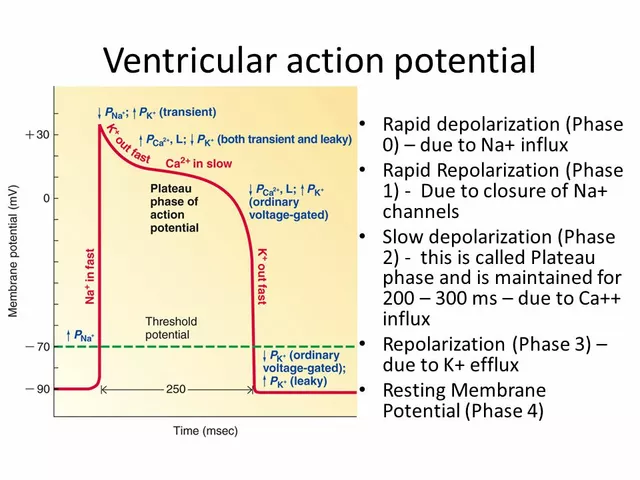
Selective serotonin reuptake inhibitors - or SSRIs - are the go-to starting point for OCD treatment. Why? Because they work, and they’re easier to tolerate. The FDA has approved several SSRIs for OCD: fluoxetine (Prozac), fluvoxamine (Luvox), paroxetine (Paxil), and sertraline (Zoloft). But here’s the catch: the doses needed for OCD are much higher than those used for depression. For example, a typical starting dose of sertraline for depression is 50 mg a day. For OCD, doctors often begin at 25 mg and slowly bump it up to 200-300 mg daily. That’s not a typo. It takes high doses to hit the target. Same with fluvoxamine: while 100 mg might help with depression, 200-300 mg is what’s needed for OCD. Fluoxetine and paroxetine follow similar patterns - 40-60 mg daily is the sweet spot. It’s not just about dosage. Timing matters too. Most people don’t see real improvement until they’ve been on the medication for 8 to 12 weeks. And even then, it’s not instant. The first two weeks often bring more anxiety, not less. That’s normal. About 37% of patients consider quitting during this early phase, but 89% of them feel better if they stick with it. Doctors use the Yale-Brown Obsessive Compulsive Scale (CY-BOCS) to track progress. A 25-35% drop in scores is considered a meaningful response. That means if someone was having 15 obsessive thoughts a day, they might drop to 10 or fewer. It’s not a cure, but it’s life-changing.Clomipramine: The OG OCD Drug
Clomipramine - sold under the brand name Anafranil - was the first drug ever approved by the FDA specifically for OCD in 1989. It’s a tricyclic antidepressant, not an SSRI. That means it affects more than just serotonin. It also blocks norepinephrine and has strong anticholinergic effects. That’s why it works - but also why it comes with a heavier side effect list. For adults, dosing starts at 25 mg a day. Every 4 to 7 days, the dose increases by 25 mg until reaching 100-250 mg daily. The maximum is 250 mg. For kids aged 10 and older, it’s 1-3 mg per kilogram of body weight, with a cap of 200-250 mg depending on the source. Elderly patients start even lower - often just 10 mg - because their bodies process the drug slower. Clomipramine has a half-life of 19-37 hours, meaning it sticks around in your system. That’s why doctors often split the dose: a smaller amount in the morning, the bigger one at night. The sedation is strong, and taking it before bed helps with sleep - and reduces next-day grogginess. Studies show clomipramine is just as effective as SSRIs in adults. In fact, one meta-analysis found it improved CY-BOCS scores by 37% in children and teens - better than sertraline or fluoxetine. But here’s the trade-off: it causes 3-5 times more side effects. Dry mouth, constipation, blurred vision, weight gain, dizziness, and heart rhythm changes (QTc prolongation) are common. Some patients gain 15-25 pounds in six months. Others say they need to drink five or six glasses of water an hour just to manage the dry mouth.SSRIs vs. Clomipramine: Which One Wins?
It’s not a simple “better or worse.” It’s about balance. For most people, SSRIs win because they’re safer and easier to live with. About 85% of first-time OCD prescriptions are SSRIs. Sertraline is the most popular - prescribed in 32% of cases - followed by fluvoxamine at 28%. They’re cheaper too. Generic SSRIs cost $350-$500 a year. Clomipramine? $800-$1,200, even with insurance. But clomipramine has its place. In treatment-resistant cases - when two or more SSRIs have failed - it’s often the next step. Studies show 40-60% of people who didn’t respond to SSRIs improve with clomipramine. Some patients swear by it. One Reddit user wrote: “Clomipramine at 175 mg stopped my checking rituals after five failed SSRIs.” Still, 43% of people who try clomipramine quit because of side effects. That’s compared to 15-18% for SSRIs. Dr. Helen Blair Simpson from Columbia puts it bluntly: “For most patients, the side effect burden outweighs marginal benefits.” Clomipramine seems to work best for contamination and cleaning obsessions at doses of 150-250 mg. SSRIs are more consistent across all OCD subtypes - checking, hoarding, symmetry, intrusive thoughts.
Dosing Is Everything
Getting the dose right isn’t guesswork. It’s science. With SSRIs, doctors don’t just pick a number. They follow a slow, structured climb. For sertraline: start at 25 mg, increase by 25 mg weekly. Reach 100 mg in 3 weeks, 200 mg by week 6-8. Fluvoxamine? Start at 25 or 50 mg, jump by 50 mg every 5-7 days up to 300 mg. Paroxetine? 20 mg daily, then 40-60 mg. Fluoxetine? 20 mg, then 40-60 mg. Clomipramine is even more precise. Start at 25 mg. Wait 4-7 days. Add 25 mg. Repeat. Most people don’t feel effects until they hit 100 mg. Full benefit often takes 10-14 weeks. That’s longer than most people expect. Many give up too soon. Monitoring is critical. Doctors check heart rhythms (ECGs) if clomipramine exceeds 150 mg. Liver enzymes are tested. Blood levels of clomipramine and its metabolite desmethylclomipramine are tracked in resistant cases. Responders typically have plasma levels between 220-350 ng/mL for clomipramine and 379 ng/mL for desmethylclomipramine.What About Augmentation?
Sometimes, you don’t need to switch. You just need to add. Since 2020, more doctors are combining a low dose of clomipramine (25-75 mg) with an SSRI. This “augmentation” strategy helps people who only partially respond to SSRIs. Research shows 35-40% of these patients get better. It’s a smart middle ground: less clomipramine means fewer side effects, but enough to boost the SSRI’s effect. This approach is growing fast. Industry analysts predict clomipramine’s role will shift from a standalone drug to a supporting player - used in smaller doses, for specific cases.What’s Next?
The field is changing. In March 2023, the FDA gave Breakthrough Therapy status to a new drug called SEP-363856. Early trials showed a 45% response rate in treatment-resistant OCD at just 50 mg a day. That’s promising. At the same time, researchers are testing psilocybin - the active compound in magic mushrooms - combined with SSRIs. Early results show 60% remission at six months, compared to 35% with SSRIs alone. It’s still experimental, but it’s moving fast. For clomipramine, scientists are testing a skin patch to deliver the drug slowly. Early data shows it works as well as the pill - but with 40% fewer side effects. That could change everything.
Real Talk: What Patients Actually Experience
On OCD-UK’s forum, 62% of 1,247 people said they tolerated SSRIs better than clomipramine. On Reddit, 78% of users who tried clomipramine said they only saw results at 150 mg or higher - but 43% quit because of side effects. Drugs.com reviews tell a mixed story. Clomipramine has a slightly higher effectiveness rating (7.2/10) than SSRIs (6.8/10). But satisfaction? Clomipramine scores 5.1/10. SSRIs get 6.2/10. People feel better - but they don’t feel good. One woman wrote: “I took sertraline for a year. My thoughts didn’t stop, but I could finally leave the house. Clomipramine made me feel like a zombie. I chose the zombie over the prison.”When to Try What
Here’s a simple roadmap:- Start with an SSRI. Pick one - sertraline or fluvoxamine are common first choices.
- Take it for 8-12 weeks. Don’t quit at 4 weeks. Wait.
- Reach the high end of the dose range. 200-300 mg for sertraline. 200-300 mg for fluvoxamine.
- If no improvement after 12 weeks, try a different SSRI. Give it another 12 weeks.
- If two SSRIs fail, talk to your doctor about clomipramine.
- If you’re a teen or older adult, start lower and move slower.
- If you’re still stuck, ask about augmentation: SSRI + low-dose clomipramine.
Final Thoughts
There’s no magic pill for OCD. But there are proven options. SSRIs are the safe, smart start. Clomipramine is the powerful backup - not for everyone, but for those who’ve run out of other choices. The key isn’t finding the best drug. It’s finding the right one for you - at the right dose, with the right support, and enough patience to let it work.Can SSRIs make OCD worse at first?
Yes, in the first 1-2 weeks, some people experience increased anxiety or more frequent obsessive thoughts. This is temporary and happens in about 37% of cases. If you keep taking the medication, symptoms improve in 89% of people. Doctors often start with lower doses (12.5 mg) and explain this phase ahead of time to help patients stay on track.
How long does it take for OCD medication to work?
Most people need 8 to 12 weeks to see real improvement. Some notice small changes by week 4, but full benefits usually take longer. For clomipramine, it can take 10-14 weeks to reach the full therapeutic dose. Patience is critical - stopping too early is the most common reason treatment fails.
Is clomipramine better than SSRIs for OCD?
In adults, studies show clomipramine and SSRIs are equally effective. But clomipramine causes more side effects - dry mouth, weight gain, dizziness, heart rhythm changes. For kids, it may be slightly more effective, but side effects are still a major concern. SSRIs are safer and easier to tolerate, so they’re recommended first. Clomipramine is reserved for cases where SSRIs don’t work.
What’s the highest safe dose of clomipramine?
The maximum daily dose for adults is 250 mg. For children aged 10 and older, the limit is 200-250 mg depending on weight and guidelines. Elderly patients should not exceed 100-150 mg. Doses above 150 mg require an ECG to check heart rhythm (QTc interval). Blood level monitoring is recommended for doses above 75 mg to avoid toxicity.
Can you take clomipramine with an SSRI?
Yes - this is called augmentation and is becoming more common. A low dose of clomipramine (25-75 mg) added to an SSRI can help people who only partially respond to the SSRI alone. Research shows 35-40% of these patients improve. This approach reduces clomipramine’s side effects while boosting effectiveness. It’s often used after two failed SSRI trials.
Are there new OCD medications coming?
Yes. A new drug called SEP-363856 received FDA Breakthrough Therapy designation in 2023 after showing 45% response rates in treatment-resistant OCD at 50 mg/day. Researchers are also testing psilocybin combined with SSRIs, with early results showing 60% remission at six months - far higher than SSRIs alone. A transdermal patch for clomipramine is in trials and may reduce side effects by 40%.
What if my insurance won’t cover clomipramine?
Generic clomipramine is often covered, but some insurers require prior authorization or step therapy - meaning you must try two SSRIs first. If denied, ask your doctor to appeal with clinical notes showing failed SSRI trials. Many pharmacies offer discount programs. The annual cost of generic clomipramine is $800-$1,200, while SSRIs cost $350-$500. If cost is a barrier, ask about lower-dose augmentation instead of full-dose clomipramine.





8 Comments
Oh wow, another 2000-word medical textbook disguised as a Reddit post. Congrats, you just wrote the OCD Wikipedia page and called it ‘real talk.’
Let me guess - you’re the guy who prints out drug monographs and brings them to therapy like it’s a Bible. Do you also measure your serotonin levels with a ruler?
And yes, of course, clomipramine is ‘just as effective’ - if you enjoy dry mouth so bad you start licking your own elbow to feel something. 37% drop in CY-BOCS? That’s like saying your prison cell got a new paint job.
Also, ‘Zombie over prison’? Wow. Deep. I’m crying. Next you’ll tell me SSRIs are just ‘emotional Velcro’ for your thoughts.
Stop romanticizing side effects. You’re not a poet. You’re a patient. And you’re not supposed to feel like a toaster that’s been left on too long.
Hey, i just wanna say this post was so helpful and i really appreciate how clear it was. I was about to quit my sertraline at 8 weeks cause i thought it wasnt working, but now i know to stick with it. I had no idea the doses were so high for ocd vs depression. My doc just said ‘take 50mg’ and i thought that was it. Turns out i needed to go up to 200mg like a total newbie. Thank you for explaining the timeline - i feel less alone now. You’re doing great. Keep going. You got this 💪
LET ME TELL YOU WHAT HAPPENED WHEN I TRIED CLOMIPRAMINE.
I WAS ON 150MG FOR 11 WEEKS. MY MOUTH WAS SO DRY I COULD HEAR MY TONGUE STICKING TO THE ROOF OF MY MOUTH LIKE A STALE GUM WRAPPER. I WENT TO THE BATHROOM EVERY 20 MINUTES JUST TO DRINK WATER. I WOKE UP AT 3AM WITH A HEART THAT FELT LIKE IT WAS BEATING THROUGH MY CHEST.
AND THEN - AND THIS IS THE CRAZY PART - I STOOD IN FRONT OF THE MIRROR AT 4AM AND REALIZED I HADN’T CHECKED THE DOOR LOCK ONCE IN 12 HOURS.
12 HOURS.
I CRIED. NOT FROM THE SIDE EFFECTS. FROM THE SILENCE.
THE OCD WAS QUIET.
But I quit anyway. Because I couldn’t stand feeling like a walking pharmacy. I didn’t want to be the guy who needs a water bottle taped to his belt. I wanted to be the guy who just… lived.
So yeah. It works. But at what cost? I’m not sure I’d do it again.
Can we talk about the lack of longitudinal data on augmentation? You mention SSRI + low-dose clomipramine works for 35-40% of non-responders, but where’s the 2-year follow-up? What’s the relapse rate? Are we just delaying the inevitable by stacking drugs?
And why no mention of CBT + medication synergy? ERP is the gold standard for OCD - yet this entire post reads like a pharmacology lecture with zero behavioral context.
Also, the claim that clomipramine is ‘better for contamination obsessions’ - source? That’s not in the 2021 meta-analysis. Are you cherry-picking?
This feels like a sponsored post disguised as lived experience. Where’s the nuance? Where’s the ‘we don’t know yet’?
So let me get this straight - the FDA approves SSRIs for OCD, but only if you take 4x the depression dose? And clomipramine? A 1989 drug that’s basically a chemical weapon with a side of constipation?
Meanwhile, the same pharma companies that pushed this are now funding psilocybin trials. Coincidence?
They don’t want you cured. They want you medicated. Forever. Because a cured patient is a lost customer.
And why are we still using 30-year-old protocols? Because the system is broken. Big Pharma owns the guidelines. Your doctor isn’t your advocate - they’re a middleman for a $200 billion industry.
Don’t trust the system. Question everything. Especially the ‘standard of care.’
The clinical data presented is accurate and well-structured. Dosing protocols for SSRIs and clomipramine align with current APA and WFSBP guidelines. The distinction between treatment response and remission is appropriately noted.
However, the omission of pharmacogenomic considerations - particularly CYP2D6 and CYP2C19 polymorphisms - limits the practical utility of this guide for personalized medicine.
Additionally, the cost comparison between generic SSRIs and clomipramine should account for pharmacy benefit manager formulary tiers, which vary significantly by region and insurer.
Recommendation: Supplement this with a discussion of therapeutic drug monitoring and genotype-guided dosing.
Bro. SSRIs are just antidepressants with extra steps. Like ordering a burger and getting 17 pickles because ‘it’s better for you.’
Clomipramine? That’s the OG. The OG that makes you feel like your tongue is made of sandpaper and your brain is running on dial-up.
And yeah, psilocybin? Sounds like a college kid’s idea of ‘healing.’ But hey, if it works, I’m all for it. At least it’s not another pill I have to swallow while my mom watches me like I’m a lab rat.
Also, why is clomipramine so expensive? Because Big Pharma hates people with OCD. Plain and simple.
Also also - did anyone else notice the article says ‘89% feel better if they stick with it’ but doesn’t say how many of those 89% are still on meds 5 years later? Just sayin’.
Life is a paradox. We seek control through chemical surrender.
SSRIs don’t cure OCD - they just make the noise quieter. Like noise-canceling headphones on a screaming toddler.
Clomipramine? That’s not medicine. That’s a spiritual trial. You don’t take it to feel better. You take it to find out if you’re still human after the side effects strip you bare.
And psilocybin? Maybe that’s not a drug. Maybe it’s a mirror. And the mirror doesn’t care if you’re ready to see yourself.
We’re not just treating symptoms. We’re trying to outsmart the architecture of our own minds.
And yet… we still take pills.
Why? Because sometimes, the only way to find peace is to let something else do the heavy lifting.
🪞