Why Hepatocellular Carcinoma Starts in Cirrhosis
Most people with hepatocellular carcinoma (HCC) already have cirrhosis. In fact, over 80% of cases develop in livers damaged by long-term scarring - whether from hepatitis B or C, heavy alcohol use, or fatty liver disease. Cirrhosis doesn’t just mean a damaged liver; it means the liver is constantly trying to repair itself, and that process can go wrong. Cells start dividing uncontrollably, and cancer takes root. That’s why finding HCC early is so critical. If caught when the tumor is still small - under 2 cm - the chances of curing it jump dramatically.
How Surveillance Works: The 6-Month Rule
Doctors don’t wait for symptoms. By the time someone feels pain, loses weight, or turns yellow, the cancer is often too advanced. Instead, guidelines from the American Association for the Study of Liver Diseases (AASLD) and the European Association for the Study of the Liver (EASL) recommend biannual ultrasound scans for everyone with cirrhosis. That’s every six months, no exceptions. Why? Because HCC tumors typically grow about 1 to 2 centimeters in that time. If you scan every six months, you catch it before it spreads.
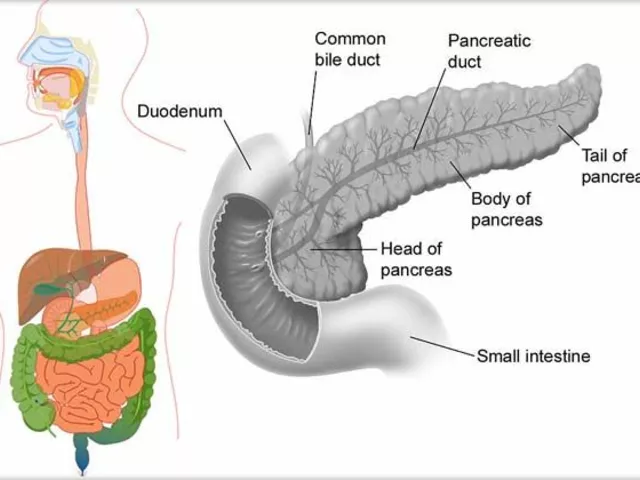
The ultrasound is simple, painless, and doesn’t use radiation. A technician moves a handheld device over your abdomen, looking for any unusual lumps. It’s not perfect - small tumors can hide behind scar tissue - but it’s the best tool we have for routine screening. Some centers add a blood test for alpha-fetoprotein (AFP), but this isn’t reliable on its own. AFP can be high in cirrhosis even without cancer, and some cancers don’t raise it at all. So, ultrasound is the main game. If something looks suspicious, the next step is always a contrast-enhanced CT or MRI scan to confirm.
Who Gets Screened? Not Everyone With Cirrhosis
It used to be simple: if you have cirrhosis, you get screened. But now, experts are getting smarter. The EASL’s 2023 Policy Statement introduced risk-based screening. Not all cirrhosis is the same. Someone with Child-Turcotte-Pugh (CTP) Class C cirrhosis - meaning their liver is failing - has a life expectancy of less than two years. Screening them for HCC doesn’t help much if they’re not going to live long enough to benefit from treatment. So, current guidelines say: skip surveillance for Class C patients unless they’re on a transplant list.
Meanwhile, people with milder cirrhosis (Class A or B) are still screened. But even among them, risk varies. Someone with hepatitis B has a 5-8% annual chance of developing HCC. Someone with fatty liver disease after successful treatment might have only a 1-3% risk. New tools like the aMAP score - which looks at age, gender, albumin, bilirubin, and platelet count - can predict risk with 81% accuracy. If your risk is below 1.5% per year, some experts argue screening may not be worth it. This shift is still being adopted, but it’s the future.
What Happens When HCC Is Found
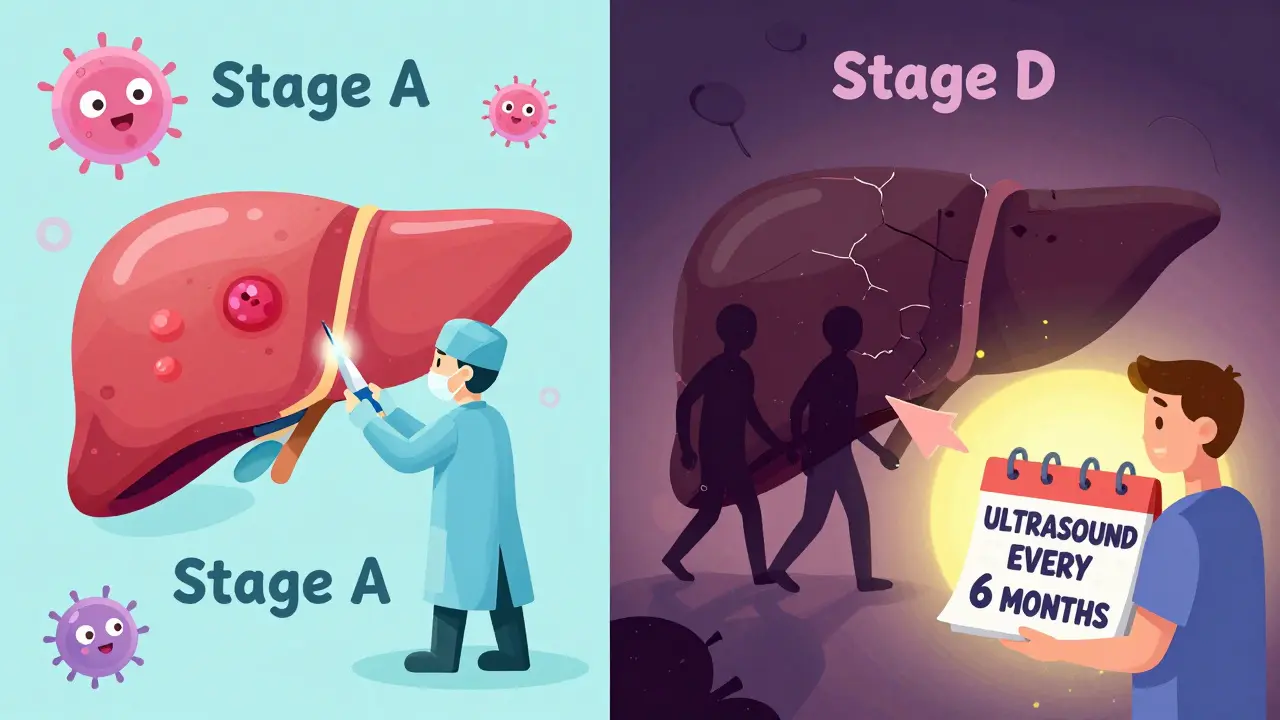
Once a tumor is confirmed, doctors use the Barcelona Clinic Liver Cancer (BCLC) staging system to decide what to do. This isn’t just about tumor size - it’s about liver function, overall health, and whether the cancer has spread.
Stage 0 or A (Early): Tumors are small, single, and the liver still works well. Treatment options here are curative. You might get a liver transplant, surgical removal, or radiofrequency ablation (RFA), where heat destroys the tumor through a needle. Success rates for these treatments can be over 70% at five years if caught early.
Stage B (Intermediate): Multiple tumors, but still confined to the liver. The go-to treatment is transarterial chemoembolization (TACE). A catheter delivers chemo directly to the tumor and blocks its blood supply. It doesn’t cure, but it can shrink tumors and extend life by years.
Stage C (Advanced): Cancer has spread to blood vessels or nearby organs. Systemic treatments like sorafenib, lenvatinib, or immunotherapy combinations (atezolizumab + bevacizumab) are used. These aren’t cures, but they can slow progression and improve survival by months.
Stage D (End-stage): Liver failure dominates. Comfort care becomes the focus. No treatment can help at this point.
The Reality of Screening: Why So Few People Get It
Here’s the hard truth: only about 40% of people with cirrhosis in the U.S. get regular HCC screening. In some communities, it’s as low as 30%. Why? For starters, many primary care doctors don’t know the guidelines. They see a patient with cirrhosis and assume someone else is handling it. Or they forget to order the ultrasound.
Patients miss appointments too. One in three doesn’t show up for their next scan. Some are scared. Others don’t understand why they need it if they feel fine. A nurse in Melbourne told me last year: “I spend 25 minutes explaining to one patient why they need this scan. Then the next patient says, ‘I’ve had a scan last year - why again?’”
There are also system problems. Only 45% of hepatology clinics have automated reminders in their electronic records. Without them, screenings slip through the cracks. Studies show that when clinics use patient navigators - staff who call, remind, and help schedule - no-show rates drop from 32% to just 14%.
New Tools on the Horizon
The next five years will change how we detect HCC. AI-assisted ultrasound tools like Medtronic’s LiverAssist are already FDA-cleared. They help radiologists spot tiny tumors that humans might miss - improving detection by up to 22%. Meanwhile, blood tests are getting smarter. The GALAD score - which combines gender, age, AFP, AFP-L3, and DCP - detects early HCC with 85% accuracy at 90% specificity. It’s not ready to replace ultrasound yet, but it could become a powerful add-on.
MRIs are also getting faster. New 5- to 7-minute liver MRI protocols are cutting costs to $350-$400. For high-risk patients - like those with hepatitis B or a family history - MRI might soon replace ultrasound as the first-line tool. The SURVIVE trial, which is tracking 10,000 patients across the U.S. and Europe, will deliver results by late 2025. It’s testing whether risk-based screening improves survival and reduces unnecessary tests.

What You Can Do
If you have cirrhosis:
- Ask your doctor for a liver ultrasound every six months - no excuses.
- Don’t wait for symptoms. By then, it’s often too late.
- Keep your liver as healthy as possible: avoid alcohol, manage diabetes, lose weight if needed.
- If you’re on a transplant list, make sure your screening is documented and up to date.
- If you’re having trouble getting scheduled, ask for a patient navigator or care coordinator.
If you’re a caregiver or family member: remind them. Write down the next appointment. Go with them. Make sure they understand why this scan matters.
Final Thought
Hepatocellular carcinoma is deadly - but not inevitable. It’s not a matter of luck. It’s a matter of catching it early. And that’s not just up to doctors. It’s up to you. If you have cirrhosis, you’re in the highest-risk group. That doesn’t mean you’ll get cancer. But it does mean you need to be vigilant. Six-month ultrasounds aren’t optional. They’re your best shot at living a full life after a cirrhosis diagnosis.
Do all people with cirrhosis need HCC screening?
Most do - but not all. Current guidelines recommend screening for all adults with Child-Turcotte-Pugh Class A or B cirrhosis. For those with Class C cirrhosis, screening is usually not recommended unless they’re on a liver transplant waiting list, because their life expectancy is too short to benefit. New risk models like the aMAP score are helping doctors decide who truly needs screening based on annual HCC risk, with thresholds set at 1.5% or higher.
What’s the best test for liver cancer screening?
Biannual abdominal ultrasound is the standard first-line test. It’s non-invasive, widely available, and effective at detecting tumors over 1 cm. Alpha-fetoprotein (AFP) blood tests are sometimes added, but they’re not reliable enough to use alone. If ultrasound shows a suspicious mass, a contrast-enhanced CT or MRI is required to confirm the diagnosis using standardized criteria like LI-RADS.
Can HCC be cured?
Yes - but only if caught early. In Stage 0 or A (small, single tumors with good liver function), treatments like surgical removal, radiofrequency ablation, or liver transplant can lead to 5-year survival rates of 60-70%. Once the cancer spreads beyond the liver or the liver function is poor, treatment shifts from cure to control. Even then, newer therapies like immunotherapy combinations can extend life by months or even years.
Why isn’t everyone getting screened for HCC?
Multiple barriers exist. Many primary care providers aren’t aware of the guidelines. Electronic health records often lack automated reminders. Patients miss appointments due to lack of understanding, transportation issues, or fear. Disparities also exist: Black patients and those on Medicaid are significantly less likely to receive screening than white, privately insured patients. Only about 40% of cirrhotic patients in the U.S. get timely screening.
Are there new blood tests for liver cancer detection?
Yes. The GALAD score - combining gender, age, AFP, AFP-L3, and DCP - detects early HCC with 85% sensitivity and 90% specificity. The aMAP score uses age, gender, albumin, bilirubin, and platelets to predict risk. These aren’t replacements for ultrasound yet, but they’re becoming valuable tools to supplement imaging, especially for high-risk patients. The HESBA alliance is currently testing 17 new biomarkers, with results expected by 2027.
How often should someone with cirrhosis get screened?
Every six months. This interval is based on how fast HCC tumors grow - typically 1 to 2 centimeters every six months in cirrhotic livers. Scanning more often doesn’t improve outcomes and increases cost and false positives. Scanning less often misses tumors before they’re treatable. Consistency matters more than frequency.
What Comes Next?
If you’re living with cirrhosis, your next step is simple: schedule your next ultrasound. Don’t wait for your doctor to remind you. Call now. If you’ve missed one in the past, get back on track. Early detection saves lives - not just in theory, but in real numbers. People are living longer because someone caught a tiny tumor on a routine scan. That could be you. And it starts with one phone call.





14 Comments
Six-month ultrasounds? More like a government scam to keep the radiology industry fat and happy. If you're that worried, get a CT. No more hand-holding.
I am a nurse in Mumbai. Many patients think if they feel fine, no scan needed. I tell them: cancer doesn't shout. It whispers. And by the time it shouts, it's too late. Ultrasound is free here. Just come.
The aMAP score? A clever distraction. The real agenda is reducing healthcare costs by denying screening to the elderly and poor. You think this is medicine? It's actuarial science disguised as clinical guidance. Watch how the insurance companies quietly adopt these thresholds.
Ah yes, the sacred six-month ultrasound. The modern-day oracle. We've replaced faith with fluoroscopy, and now we bow before the god of imaging. How quaint. The liver doesn't care about your algorithm. It just wants to be left alone.
Thank you for this meticulously researched and clinically grounded overview. The distinction between Child-Pugh classes is critical, and the emphasis on patient navigation as a systemic intervention is both evidence-based and profoundly humane. I will be sharing this with our clinic's quality improvement committee.
Is the GALAD score available outside the US? In India, most labs don't test for AFP-L3 or DCP. Is there a cheaper alternative we can use?
I mean, if you're gonna get scanned every six months, why not just skip the ultrasound and go straight to the MRI? Like, if you're rich enough to have cirrhosis, you're rich enough to afford a $400 scan. Right?
I work with refugees in Chicago, and this article? It's a lifeline. Many don't know what cirrhosis even means, let alone that they need a scan. We now hand out laminated cards with the six-month rule in Spanish, Arabic, and Somali. One woman cried when she realized she could live longer just by showing up. That's not medicine. That's dignity.
My dad had cirrhosis from alcohol. He skipped his scans for two years. Said he didn't want to know. He died at 58. I wish someone had told him the truth: it's not about the cancer. It's about the chance.
Just go get the scan. No excuses. Your liver doesn't care if you're busy or scared. It just wants you to show up. One phone call. That's all. Do it for yourself
I had hepatitis B and thought I was fine. Then I got my scan and found a 1.2 cm tumor. RFA worked like magic. I'm alive today because I listened. Don't wait like I did. Your future self will thank you.
If you have cirrhosis and you're not getting scanned every six months you're playing Russian roulette with your liver and you know it. Stop making excuses. Your life is worth more than your fear
so i heard the fda approved some ai thing for liver scans but the real story is the gov is using it to cut medicaid spending?? like why else would they push this??
I find it deeply unsettling that we have reduced the sanctity of human life to a statistical threshold - a 1.5% annual risk is deemed 'insufficient' to warrant intervention. What a chilling, utilitarian vision of care. I weep for the future of medicine.