When you’re prescribed an antibiotic like azithromycin or clarithromycin for a stubborn chest infection, you probably don’t think about your heart. But these common drugs can quietly mess with your heart’s rhythm - and in some people, that’s dangerous. The risk isn’t high for most, but for a small group, it can mean the difference between a quick recovery and a trip to the emergency room. The question isn’t whether macrolides are safe - they are, for most. The real question is: who needs an ECG before taking them?
Why Macrolides Can Affect Your Heart
Macrolide antibiotics - azithromycin, clarithromycin, and erythromycin - work by stopping bacteria from making proteins. But they also block a specific potassium channel in heart cells called hERG. When that channel gets blocked, the heart takes longer to reset between beats. On an ECG, that shows up as a longer QT interval. A prolonged QT interval doesn’t cause symptoms by itself. But it can trigger a rare, life-threatening arrhythmia called Torsades de Pointes. This isn’t a theoretical risk. A 2012 study in the New England Journal of Medicine found that people taking azithromycin had a 2.7 times higher risk of dying from heart problems than those taking amoxicillin. Erythromycin carries the highest risk, followed by clarithromycin. Azithromycin is the safest of the three, but it’s also the most commonly prescribed.The absolute risk of Torsades is low - about 1 to 8 cases per 10,000 people per year. But when the QT interval stretches beyond 500 milliseconds, the risk jumps to 3-5%. For every 10 extra milliseconds beyond that, the risk goes up another 5-7%. That’s not a small increase. It’s a red flag.
Who’s at Highest Risk?
Not everyone needs an ECG before starting a macrolide. But if you have any of these risk factors, you’re in the group that should be screened:- Women - female sex doubles the risk (relative risk 2.9)
- Age 65 or older - risk increases 2.3 times
- Existing heart conditions - heart failure, prior arrhythmias, or a history of QT prolongation
- Low potassium or magnesium levels - often from diuretics or poor diet
- Other QT-prolonging drugs - antidepressants like citalopram, antifungals like fluconazole, or even some anti-nausea meds
- Chronic kidney disease - macrolides build up in the body if kidneys aren’t clearing them
- Family history of sudden cardiac death or Long QT Syndrome
One or two of these? You’re in the gray zone. Three or more? You need an ECG before starting the antibiotic. A 2025 analysis from the NIH showed that when all these factors are combined, the actual risk of arrhythmia drops to near background levels - meaning the drug itself isn’t the main culprit. It’s the combination.
When ECG Monitoring Is Required
The British Thoracic Society (BTS) set the gold standard in 2020: anyone starting long-term macrolide therapy for respiratory conditions like bronchiectasis or COPD must have a baseline ECG. That’s because these patients often take macrolides for months or years - and the risk builds up over time. The cutoff? QTc over 450 ms for men, over 470 ms for women. If it’s higher than that, don’t start the drug.For short-term use - say, a 5-day course of azithromycin for a sinus infection - the rules are looser. But even then, if you’re over 65, on multiple meds, or have kidney issues, an ECG makes sense. The problem? Most GPs don’t do it. A 2024 survey of 247 UK primary care doctors found that only 22% routinely ordered ECGs before prescribing macrolides. Why? Time, lack of clear guidelines for acute cases, and the belief that healthy people are fine.
But here’s the catch: many patients aren’t as healthy as they seem. In one UK clinic, 1.2% of patients screened for macrolide therapy were found to have undiagnosed Long QT Syndrome. That’s one in every 80 people. Without screening, that person could have taken azithromycin and collapsed.
What Happens If You Skip the ECG?
In hospital settings, where monitoring is routine, the system works. Nurses check ECGs before giving IV erythromycin. Pharmacists flag interactions. If QT prolongation shows up, the drug is stopped. But outside the hospital? It’s a gamble.There’s a documented case from a Reddit thread in March 2025: a 68-year-old woman with a baseline QTc of 480 ms - just above the limit - was given clarithromycin for pneumonia. Five days later, she went into Torsades de Pointes. She needed emergency cardioversion. She survived. But she could have died. Her ECG had been done a year earlier for a different reason. No one checked it again.
Another study found that in primary care, only 12% of patients on macrolides had any ECG monitoring - compared to 87% in specialist respiratory clinics. The gap isn’t about knowledge. It’s about systems. Most GPs don’t have easy access to ECG machines. They don’t have time to wait 3-7 days for results. And they’re not trained to interpret borderline QT values.
How ECG Monitoring Actually Works
If you’re being screened, here’s what happens:- Before your first dose, you get a 12-lead ECG. It takes 5 minutes.
- A trained person measures the QT interval and corrects it for heart rate (QTc). This isn’t automatic - many machines give inaccurate readings.
- If QTc is under 450 ms (men) or 470 ms (women), you’re cleared.
- If it’s between 450-499 ms, your doctor should review your other risk factors. They might still prescribe it but with caution.
- If it’s over 500 ms, the drug is avoided. Alternative antibiotics like doxycycline or amoxicillin are used.
- For long-term users, a repeat ECG is done at one month to catch new prolongation.
Some UK clinics are now using point-of-care devices that give results in under 2 minutes. One pilot program cut the delay in starting therapy from 5.2 days to just 0.8 days. That’s a game-changer for patients who need to start treatment fast.
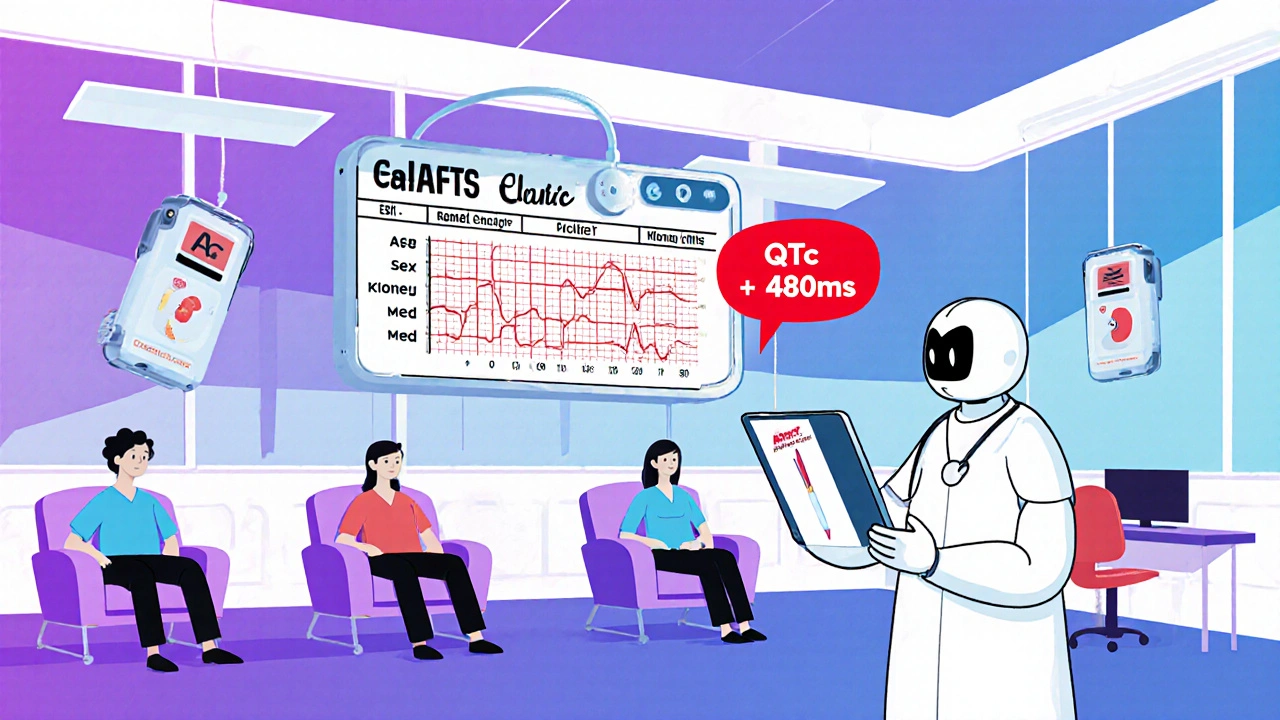
What About Electronic Alerts?
The future is in tech. By early 2025, 43% of U.S. hospitals using Epic EHR systems had automated alerts that pop up when a doctor tries to prescribe azithromycin to someone with a known long QT or on other QT-prolonging drugs. The system checks the patient’s last ECG, their meds, and their age. If the risk is high, it says: “Consider alternative antibiotic. ECG recommended.”These alerts aren’t perfect - they generate false positives. But they’ve cut prescribing errors by 31% in places where they’re used. In the UK, NHS Digital is testing similar systems. The goal isn’t to replace clinical judgment. It’s to remind busy doctors: “Don’t forget to check.”
The Bottom Line: Who Gets an ECG?
You don’t need an ECG if you’re a healthy 30-year-old with no heart issues, no other meds, and you’re getting a 5-day course of azithromycin for a simple infection.You do need one if:
- You’re over 65
- You’re a woman with any heart risk factor
- You’re on diuretics, antidepressants, or antifungals
- You have kidney disease
- You’re starting long-term macrolide therapy (3+ weeks)
- You’ve had a fainting episode or unexplained cardiac arrest in your family
And if you’re unsure? Ask your doctor: “Could this antibiotic affect my heart? Should I get an ECG?” It’s not a dumb question. It’s a smart one.
What Happens If Your QT Is Prolonged?
If your ECG shows a prolonged QT interval, your doctor won’t just stop the macrolide. They’ll look at the whole picture:- Can you switch to a different antibiotic? Amoxicillin, doxycycline, or cefdinir are safer options.
- Can you fix electrolyte imbalances? Potassium or magnesium supplements might help.
- Are you on other QT-prolonging drugs? Maybe one can be stopped or changed.
- Do you have an inherited condition? You might need a referral to a cardiologist.
Stopping the macrolide is the first step. But the real win is catching a hidden problem before it causes harm.
What’s Changing in 2025?
The American Heart Association updated its guidelines in April 2025 to recommend a 9-point risk score for macrolides. Points are added for age, sex, kidney function, meds, and more. If you score 4 or higher, get an ECG. If you score 7+, avoid macrolides entirely.Cost is still a barrier. An ECG in the UK costs about £28.50. If every macrolide prescription got one, it would cost £342 million a year. That’s not feasible. But targeting high-risk patients? That’s where the savings are. The Institute for Clinical and Economic Review estimates that smart screening could save the U.S. healthcare system $217 million a year by preventing arrhythmias and hospitalizations.
It’s not about checking everyone. It’s about checking the right people.
Do all macrolide antibiotics carry the same heart risk?
No. Erythromycin has the highest risk of QT prolongation, followed by clarithromycin. Azithromycin carries the lowest risk among the three, but it’s still capable of causing arrhythmias - especially in people with multiple risk factors. Even though azithromycin is the most commonly prescribed, its safety profile is relative, not absolute.
Can I take azithromycin if I have a mild QT prolongation?
If your QTc is between 450-499 ms, your doctor may still prescribe azithromycin if you have no other risk factors and are otherwise healthy. But they should monitor you closely. If you’re over 65, on other meds, or have kidney disease, they’ll likely choose a different antibiotic. Never ignore a borderline QT result.
How long after starting a macrolide can heart problems happen?
Most cases of Torsades de Pointes occur within the first 3-5 days of starting the drug. That’s why monitoring is most critical early on. But with long-term use, risk can build up over weeks. That’s why repeat ECGs at one month are recommended for patients on macrolides for more than two weeks.
Is an ECG the only way to check for QT prolongation?
Yes. No blood test, symptom, or wearable monitor can reliably detect QT prolongation. Only a 12-lead ECG with accurate measurement of the QT interval - corrected for heart rate (QTc) - can confirm it. Some smartwatches claim to detect arrhythmias, but they can’t measure QT intervals accurately enough for clinical decisions.
What should I do if I feel dizzy or have palpitations while on a macrolide?
Stop taking the antibiotic and seek medical attention immediately. Dizziness, palpitations, or fainting could be signs of a dangerous heart rhythm. Don’t wait to see if it passes. Call your doctor or go to the nearest emergency department. Bring your medication list with you - it’s critical for diagnosis.
Are there safer antibiotics than macrolides for people at risk?
Yes. For many infections, amoxicillin, doxycycline, cefdinir, or levofloxacin (with caution) are safer alternatives. The choice depends on the infection type. Your doctor should weigh the risk of the antibiotic against the risk of not treating the infection. Never assume macrolides are the only option.






12 Comments
I never realized how many people are walking around with undiagnosed Long QT. My aunt had a fainting episode at 62 and they never connected it to her meds. She got azithromycin for bronchitis and ended up in the ER. Turned out her QTc was 510. No one checked. No one asked. Just another 'lucky' survivor.
Actually, the risk is even higher in South Asian populations due to higher prevalence of subclinical electrolyte imbalances and CYP3A4 polymorphisms. Most studies are based on Western cohorts, so global guidelines are dangerously outdated. We need region-specific thresholds, not just gender-based ones.
Let’s be real: the entire system is a farce. We’re told to 'trust the science'-but the science is built on fragmented, underpowered studies, and then weaponized by pharmaceutical marketing departments. Azithromycin is cheap, convenient, and profitable. ECGs? Too expensive. Too inconvenient. Too human. We’d rather gamble with a 1 in 10,000 chance than invest 28 quid and five minutes. And then we call it 'medical progress.'
It’s not about the drug. It’s about the system that rewards speed over safety. And until we stop pretending that efficiency equals efficacy, people will keep dying in their living rooms while their GP clicks 'approve' on a prescription.
Oh wow, another 'you need an ECG' post. Let me guess-this is from someone who thinks every 65-year-old with a cough needs a cardiologist on speed dial? I’ve worked in primary care for 12 years. The vast majority of these patients are fine. We’re pathologizing normal aging. If you’re on 12 meds and have kidney disease, sure, check your QT. But for the average person? Stop fear-mongering. Azithromycin isn’t poison. It’s a tool. Use it wisely, not with panic.
My dad took clarithromycin after his pneumonia and had a near-miss. He didn’t even know he had high blood pressure until then. Now he’s on a beta-blocker and gets ECGs every time he gets antibiotics. I’m so glad we caught it. If you’re even a little unsure-ask. Seriously. It’s not being paranoid. It’s being smart.
Hey everyone, I work in a rural clinic in India and we’ve started using handheld ECGs for anyone over 55 on macrolides. It’s changed everything. We used to just prescribe and hope. Now we catch 2-3 borderline QT cases every month. One guy had undiagnosed hypertrophic cardiomyopathy. Another had low potassium from diuretics he didn’t tell anyone about. These devices cost less than a coffee. Why aren’t we using them everywhere? We can’t wait for big hospitals to lead. We have to start where we are.
It’s funny how we treat antibiotics like candy. We pop them like Advil and act shocked when something goes wrong. But the heart? The heart doesn’t care if you're 'generally healthy.' It just responds to chemistry. That potassium channel doesn’t negotiate. It doesn’t care if you're 30 or 80. It just does its job-until it doesn’t. Maybe the real question isn’t who needs an ECG. It’s why we’re so afraid to look before we leap.
So we’re supposed to get an ECG for every azithromycin script? Cool. Meanwhile, my doctor still won’t prescribe me a refill for my blood pressure med because 'it’s not urgent.' Funny how we’ll spend $30 to prevent a 0.01% risk but won’t spend $5 to keep someone alive today.
Let’s not pretend this is about patient safety. It’s about liability. Hospitals don’t want to be sued when someone drops dead after a 5-day course. So they push ECGs on the high-risk group-not because it’s medically perfect, but because it’s legally defensible. The real problem? We’ve outsourced clinical judgment to algorithms and checklists. And now we’re surprised when doctors don’t think anymore.
Why are we letting big pharma dictate our protocols? Azithromycin is a generic. ECGs cost more. So the system favors the drug. If it was a brand-name drug with a patent, we’d be doing ECGs on everyone. Wake up. This isn’t medicine. It’s economics.
Just got my first handheld ECG last month. Took 90 seconds. Showed QTc 482. Doc switched me to doxycycline. No big deal. I’m alive. My grandma didn’t get one. She passed from torsades last year. Don’t be her. Ask. Get checked. It’s not a hassle-it’s a gift to your future self.
My doc skipped the ECG. I felt weird on day 3. Went to urgent care. QT was 508. Saved my life. Don’t wait. Ask. Simple.