Hyperuricemia: What It Is and How to Manage It
Hyperuricemia means you have too much uric acid in your blood. High uric acid itself doesn't always cause symptoms, but it raises your risk for gout, kidney stones, and long-term kidney damage.
How does uric acid build up? Your body makes uric acid when it breaks down purines — substances in many foods and in your cells. Causes include a purine-rich diet (red meat, organ meat, shellfish), sugary drinks with fructose, excess alcohol, being overweight, certain medicines, and reduced kidney clearance. Genetics also play a big role for many people.
Spotting the signs
Most people with mildly high uric acid feel fine. Warning signs include sudden, severe joint pain and swelling (usually the big toe), frequent gout attacks, blood in the urine or colicky flank pain from kidney stones, and steadily worsening kidney function. If you have these symptoms, get tested.
Diagnosis is simple: a blood test measures serum uric acid. Labs often flag levels above about 6.8 mg/dL as elevated. For treatment goals, doctors usually aim for less than 6 mg/dL in people with gout. Your provider may also order urine tests or imaging if stones or kidney problems are suspected.
Practical steps to lower uric acid
Start with lifestyle moves you can control. Cut sugary drinks and fruit juices, limit beer and spirits, and avoid organ meats and shellfish. Swap red meat for chicken or plant proteins, drink more water, and lose weight gradually if needed. Even a 5–10% weight drop can help.
If lifestyle changes don’t bring uric acid down or you have gout or stones, medications are common. Allopurinol and febuxostat reduce uric acid production. Probenecid helps your kidneys excrete more uric acid. For severe, treatment-resistant cases, biologic options like pegloticase exist but are used rarely and under specialist care.
Medication choice depends on other health issues. Allopurinol can cause a rash and rarely severe reactions; febuxostat has been linked to higher heart-related risks in some studies; probenecid doesn’t work well if kidney function is poor. Talk to your doctor about pros and cons and necessary blood tests.
When starting uric acid–lowering therapy, doctors often give a low-dose anti-inflammatory (colchicine or NSAID) for a few months to prevent gout flares triggered by changing uric acid levels. Regular follow-up testing helps keep treatment on target and safe.
Final practical tip: keep a simple log of foods, drinks, and attacks for a few months. That data helps your clinician spot triggers and tailor treatment. If you have recurrent gout, kidney stones, or a family history of high uric acid, ask for an evaluation — early steps can prevent big problems later.
Plan routine checks every 3–12 months depending on treatment and kidney health. Check liver and kidney labs when on medications. Avoid high-dose vitamin C or weight loss extremes without advice. If you're unsure about online pharmacies or generic vs brand options for uric acid drugs, bring questions to your pharmacist or doctor. Early answers save time and pain.
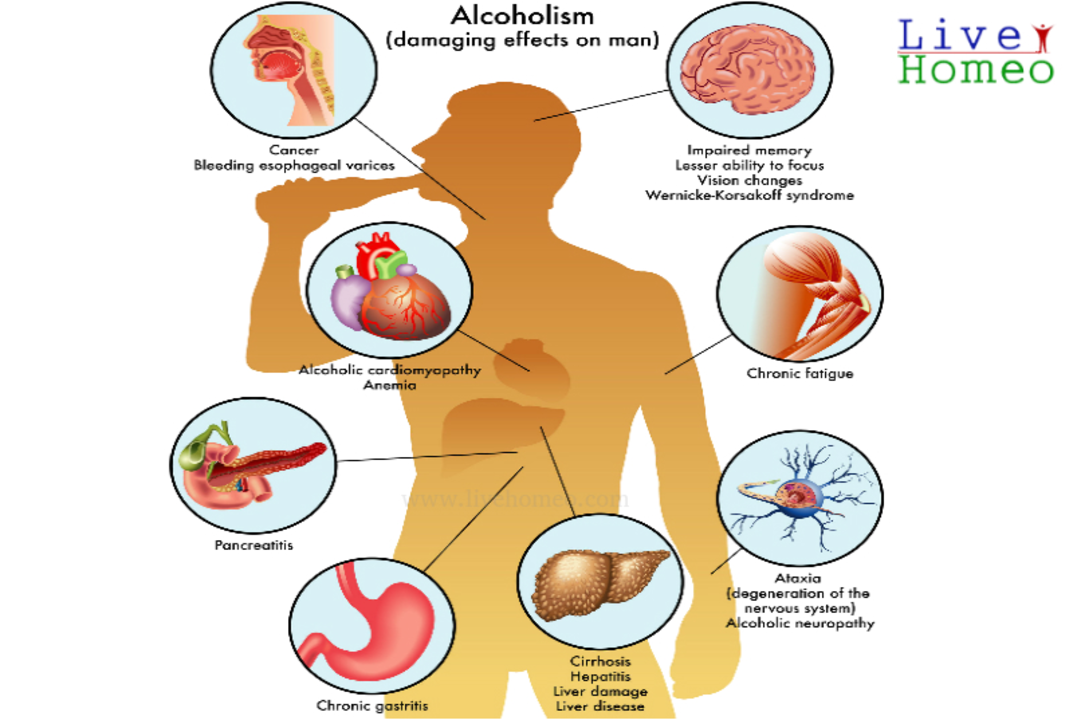
The relationship between alcohol consumption and high uric acid levels
In a recent study, I discovered a significant correlation between alcohol consumption and increased uric acid levels. As I delved deeper, I learned that excessive alcohol intake can lead to a higher production of uric acid in the body, potentially causing gout and other health issues. Interestingly, different types of alcoholic beverages like beer and liquor have varying impacts on uric acid levels. It's essential to be mindful of our alcohol consumption and consider moderation to maintain a healthy uric acid balance. I'll continue to explore this topic and share more findings to help us make informed decisions about our health and lifestyle choices.
Keep Reading